Steroid refractory acute GVHD (SR-aGVHD) occurs frequently and affects transplant outcomes adversely associated with high morbidities and mortalities. The present study attempted to develop a risk model predicting the risk of SR-aGVHD using both candidate single nucleotide polymorphism (SNP) and clinical risk factors.
A total of 268 patients were included who had diagnosis of acute GVHD and treated with systemic steroids. SR-aGVHD was defined with followings: 1) progression of GVHD after 3 days of systemic steroids; 2) No change after 7 days treatment; 3) incomplete response after 14 days of treatment initation.
Patients were randomly divided into training (n=180) and validation sets (n=88) adjusted for the presence of SR-aGVHD, disease risk, grade 3/4 aGVHD, presence of gastrointestinal and liver involvement. A total of 259 SNPs in 53 genes were genotyped as previously described (Kim, Transplantation 2012). Clinical risk factors were also included to generate risk model for SR-aGVHD.
Overall, 132 (47.3%) patients developed SR-aGVHD which was equally distributed in training and validation sets.
In the training set, 85 patients (47.2%) developed SR-aGVHD. In univariate analysis, gut involvement (p<0.0001) and grade 3/4 aGVHD (p<0.0001) were identified as risk factors as well as donor genotypes of IL6 (rs1800797; p=6.15x10-4) and IFNG (rs2069727; p=4.37x10-4). Multivariate analysis confirmed that these two SNPs along with gut GVHD were independent risk factors for SR-aGVHD, but not grade 3/4 acute GVHD.
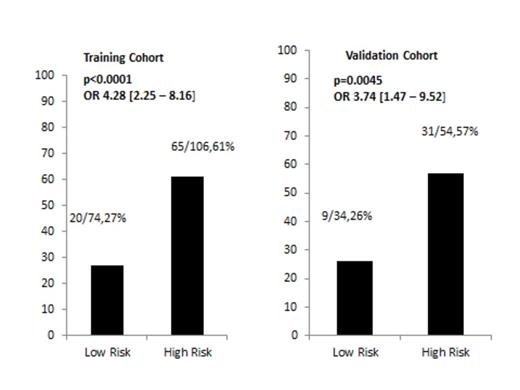
A combined risk model was generating using 2 SNPs of IL6 (rs1800797), IFNG (rs2069727) and clinical risk factor of gut GVHD. A score of one was assigned to each of above risk factors and patients were divided based on these scores. Overall, the risk of SR-aGVHD increased as scores increased. Then we divided the patients into low risk (score 0, n=74) versus high risk groups (score 1, 2 and 3, n=106). Higher incidence of SR-aGVHD was noted in high risk group (61.3%; 65/106) vs low risk group (27%; 20/74; p<0.0001, OR 4.28 [95% CI 2.25-8.16]). The combined risk model was successfully replicated to stratify the groups risk of SR-aGVHD in the validation set (p=0.0045, OR 3.74 [95% CI 1.47-9.52]): incidence of SR-aGVHD was 57% in high risk group (31/54) vs 26% low risk group (9/34) in the validation set.
When the combined risk model was used, using SNPs along with clinical risk factor, the risk model showed AUC of 0.738 in training set with sensitivity of 76 % and specificity of 56%. In the validation set, it showed AUC of 0.773 with sensitivity of 77 % and specificity of 52%.
The present study suggested that this risk model could identify high risk patient for SR-aGVHD with following information including donor genotype of IL6 (rs1800797) and IFNG (rs2069727) with gut involvement of GVHD.
The proportion of SR aGVHD according to combined risk model by diving patients into low risk (score 0) versus high risk (score 1-3) patients.
The proportion of SR aGVHD according to combined risk model by diving patients into low risk (score 0) versus high risk (score 1-3) patients.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal