Platelet engraftment is an important marker of successful allogeneic stem cell transplantation and platelet is the last to be regenerated in bone marrow after stem cell transplantation. Especially, platelet engraftment is far slower in reduced-intensity conditioning regimen(RIC) in cord blood transplant(CBT). Early prediction of platelet engraftment in RIC-CBT can be helpful to proper treatment. Recent retrospective studies suggested immature platelet fraction(IPF) can be useful to predict platelet engraftment. However, the role of IPF in RIC-CBT is not be sufficiently investigated. In addition, these studies included patients undergoing bone marrow or peripheral blood transplantation. Therefore, we analyzed cases in our database to evaluate the impact of IPF and Reticulocyte count(RET%) on the outcome of platelet engraftment in consecutive patients who were treated with RIC-CBT over the past 4 years at our institution in Tokyo, Japan.
We included 53 consecutive patients treated at our institution between April 2008 and May 2013. The study population consisted of 29 male and 23 female patients with a median age of 57 years old (range: 36-69). Patient in this cohort underwent RIC-CBT as a part of therapy for myeloid malignancies(N=28) and lymphoid malignancies (N=24). 21 patients were treated with Flu+Cy+TBI(2gy), and 31 patients were treated with Flu+Bu+TBI(2Gy). All patients received calcineurin inhibitor plus MMF for GVHD prophylaxis. Due to the influence of blood transfusion on IPF and RET% and overall estimation of IPF and RET% movement, IPF and RET% were assessed by using the 5-day moving average ,and then we compared movement of the fifth moving average between patients with platelet engraftment and patients without platelet engraftment. The fifth moving average was calculated from the time of day4 after transplantation until the date of platelet engraftment or death from any cause or the date on which the patient was received next chemotherapy. Platelet engraftment was defined as independent from platelet transfusion.
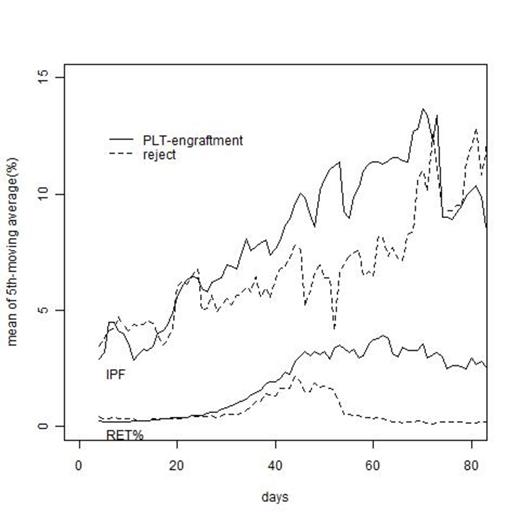
Among 53 patient, 29 patieunt achieved platelet engraftment. The median time of platelet engraftment was day +42 (range:24-203day), and median time of follow up periods of patients without platelet engraftment was 47 days. 16 patients achieved platelet engraftment after day +40. Baseline characteristics according to patients who achieved platelet engraftment, or did not achieve were similar among RIC-regimen, patient diagnosis. Patients' age, sex, total cell count andCD34 cell count in donor cord blood has no impact on pletelet engraftment. Maximum value of IPF did not have significant impact on platelet engrafment. As shown figure 1, The mean of the 5-day moveing average in IPF show similar curve from day +4 to day +30 between patient with platelet engraftment and without, and after +30 days the curve of patient with platelet engraftment gradually highter than the curve of patient without platelet engraftment. The difference of these curves was larger after day +50. In the RET% case, it was almost same. the 5-day moveing average of IPF and RET% in platelet engraftment patient were raising after day +40, while those in non-engraftment patient were decreasing in this period. Provided the 5-day moving average of IPF are blow 6.0 from day +40 to day +50, It is highly likely that platelet engraftment can't be expected (p=0.001 in univariate analyses). Likewise, provided the 5-day moving average RET% are blow 1.5 from day +40 to day +50, platelet engraftment significantly can't be expected (p=0.002).
The results of the present study highlighted the importance of the fifth-moving average of IPF and RET% after day +40, and IPF and RET% can be useful tools to predict platelet engraftment in RIC-CBT.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal