Abstract
The international prognostic index (IPI) was first described in 1993 by Shipp et al and is the most commonly used prognostication tool in DLBCL. The IPI combines 5 poor prognostic parameters (age >60 years, elevated LDH, performance status ≥2, stage III/IV and >1 site of extranodal disease). Use of the age-adjusted IPI (AA-IPI) is recommended for patients<60 years for whom 3 risk factors (stage III/IV, performance status and elevated LDH) were independently significant in the original analysis. Ziepert et al confirmed that the IPI remains a valid predictor of outcome in aggressive CD 20 positive B-cell non-Hodgkin lymphoma in the rituximab era, however the presence of >1 extranodal site of disease was no longer prognostic. In this analysis, we explored the prognostic implications of individual IPI parameters including >1 site of extranodal disease in the context of a large randomized phase III study.
The R-CHOP 14 versus 21 phase 3 open-label randomised controlled trial has been previously reported [Cunningham et al, The Lancet, Volume 381, Issue 9880, p1817-1826]. 1080 patients were randomly assigned to receive six cycles of R-CHOP every 14 days plus 2 cycles of rituximab (R-CHOP-14) or eight cycles of R-CHOP every 21 days (R-CHOP-21).
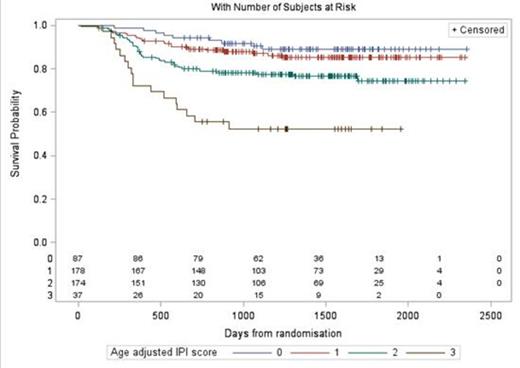
A multivariate analysis of prognostic factors was also undertaken, including age (continuous variable), gender, stage (I-IV), performance status (PS; 0 vs 1 vs 2), lactate dehydrogenase (LDH) concentration (normal vs elevated), presence or absence of B symptoms and number of extranodal sites (<1 vs >1). We particularly wished to assess whether >1 site of extranodal disease is an independent prognostic factor in our dataset, both in all treated patients (n=1071) and in those<60 years (n=473). A comparison of overall survival (OS) between the standard IPI and AA-IPI groupings was performed in patients<60 years using the Kaplan Meier (KM) method.
In multivariate analysis increased age, stage, and PS, as well as raised LDH and presence of B symptoms were associated with poor OS. Whilst >1 site of extranodal disease was not found to be independently prognostic, it was associated with a non-significant trend towards poorer OS (HR 1.312, p=0.057). When the analysis was restricted to patients<60 years, >1 extranodal site of disease was found to be associated with a significantly worse OS (HR 2.19, p=0.0025). This is in contrast to the original age-adjusted IPI which did not find >1 extranodal site to be a relevant prognostic factor in the<60 years group.
Table 1 displays the effects of >1 extranodal site on OS and PFS. OS in patients<60 years according to standard IPI and AA-IPI are shown in figures 1 and 2. Using the AA-IPI (which excludes weighting for number of extranodal sites) the poorest prognostic group have a 2 yr OS of 55%. Using the standard IPI in the same population there appears to be better differentiation of prognostic groups with the poorest prognostic group having a 2 yr OS of 40%.
Prognostic significance of >1 extranodal site of disease in multivariate analysis (OS and PFS)
| . | PFS . | OS . | ||||
|---|---|---|---|---|---|---|
| . | HR . | 95% CI . | P value . | HR . | 95% CI . | P value . |
| All patients (n=1080) | ||||||
| Univariate | ||||||
| Multivariate | 1.245 | 0.963-1.611 | 0.0948 | 1.312 | 0.983-1.753 | 0.0657 |
| <60 years patients (n=473) | ||||||
| Univariate | ||||||
| Multivariate | 1.801 | 1.178-2.755 | 0.0067 | 2.197 | 1.320-3.656 | 0.0025 |
| . | PFS . | OS . | ||||
|---|---|---|---|---|---|---|
| . | HR . | 95% CI . | P value . | HR . | 95% CI . | P value . |
| All patients (n=1080) | ||||||
| Univariate | ||||||
| Multivariate | 1.245 | 0.963-1.611 | 0.0948 | 1.312 | 0.983-1.753 | 0.0657 |
| <60 years patients (n=473) | ||||||
| Univariate | ||||||
| Multivariate | 1.801 | 1.178-2.755 | 0.0067 | 2.197 | 1.320-3.656 | 0.0025 |
Age-adjusted IPI score and overall survival in patients<60years (n=476)
In our cohort of over 1000 patients from a randomized prospective phase III trial >1 extranodal site of disease was found to be associated with a significantly worse OS in patients<60 years with DLBCL. The use of the standard IPI was superior to the age-adjusted IPI in prognostication for patients<60 years in our dataset. Extranodal disease should be identified as a priority at baseline using modalities such as PET, to assign patients to the correct prognostic group. Accurate identification of poor risk patients will help to improve our understanding of their disease biology and guide future therapeutic strategies.
Cunningham:Novartis: Research Funding; Astra-Zeneca: Research Funding; Merck KGA: Research Funding; Celgene: Research Funding; Sanofi-Aventis: Honoraria, Membership on an entity’s Board of Directors or advisory committees, Research Funding; Amgen: Consultancy, Membership on an entity’s Board of Directors or advisory committees, Research Funding; Merck: Honoraria, Membership on an entity’s Board of Directors or advisory committees; Roche: Honoraria, Membership on an entity’s Board of Directors or advisory committees, Research Funding. Hawkes:Roche: Travel expenses Other. Jack:Roche: Research Funding; Genentech: Research Funding. Pocock:Roche: Membership on an entity’s Board of Directors or advisory committees, Travel expenses Other; Pfizer: Membership on an entity’s Board of Directors or advisory committees. Ardeshna:Roche: Honoraria, Research Funding. Radford:Roche: Consultancy; Bayer-Schering: Consultancy; Millenium Pharmaceuticals: Consultancy, Research Funding; Napp Pharmaceuticals: Consultancy; Novartis: Consultancy; GlaxoSmithKline: Consultancy. McMillan:Roche: Consultancy, Honoraria, Research Funding, Travel expenses Other. Davies:Roche: Consultancy, Travel expenses Other. Turner:Roche: Travel expenses Other. Johnson:Roche: Membership on an entity’s Board of Directors or advisory committees, Travel expenses Other. Linch:Roche: Honoraria, Membership on an entity’s Board of Directors or advisory committees, Research Funding; Chugai Pharma: Honoraria, Membership on an entity’s Board of Directors or advisory committees, Research Funding; Amgen: Membership on an entity’s Board of Directors or advisory committees; Hospira: Membership on an entity’s Board of Directors or advisory committees; Celgene: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal