Abstract
Ruxolitinib is a potent JAK1/JAK2 inhibitor that has demonstrated rapid and durable reductions in splenomegaly, improved MF-related symptoms and quality of life (QoL), and prolonged survival in 2 phase 3 studies comparing ruxolitinib with placebo (COMFORT-I) and best available therapy (COMFORT-II). However, no clinical trial in pts with MF had been conducted in Asian countries, and only a limited number of Asian pts or healthy volunteers had been enrolled in any ruxolitinib study.
This study was an open-label phase 2 study evaluating ruxolitinib in Asian pts with PMF, PPV-MF, or PET-MF who had palpable splenomegaly ≥ 5 cm below the costal margin and intermediate-2– or high-risk MF by the International Working Group for Myelofibrosis Research and Treatment (IWG-MRT) criteria. Pts received starting doses of ruxolitinib 15 or 20 mg twice daily (bid) based on baseline platelet count (100-200 or > 200 × 109/L, respectively); dose adjustments balancing safety and efficacy were allowed to titrate each pt to their most appropriate dose. The primary endpoint was met if the proportion of pts achieving ≥ 35% reduction in spleen volume from baseline at week 24 was ≥ 27.5% as measured by MRI/CT. Symptomatic response was assessed as a secondary endpoint using the 7-day modified MF Symptom Assessment Form (MFSAF) v2.0 total symptom score (TSS) and European Organisation for Research and Treatment of Cancer QoL Questionnaire Core 30 (EORTC QLQ-C30). The study was conducted in China (n = 63), Japan (n = 30), Korea (n = 17), and Taiwan (n = 10). The data cutoff date for this analysis was 7 June 2013.
Overall, 120 pts were enrolled (PMF, n = 80; PPV-MF, n = 21; PET-MF, n = 19), and their baseline characteristics were as follows: median age, 61 years (range, 25-80 years); 51.7% female; 69.2% intermediate-2 and 30.8% high risk by IWG-MRT criteria; median palpable spleen size, 15 cm (range, 5-45 cm); median spleen volume, 2159 cm3; 55.8% of pts had prior exposure to hydroxyurea. The median follow-up was 8.44 months; 22.5% of pts discontinued treatment, primarily for adverse events (AEs; 9.2%) and disease progression (7.5%). The median duration of treatment was 8.44 months (range, 0.5-21.7 months), and the median daily dose was 20.64 mg/day in the 15 mg bid group (n = 46) and 36.11 mg/day in the 20 mg bid group (n = 74). All pts were evaluable for achievement of the primary endpoint, 101 pts remained on study and were evaluable at week 24, and 96 pts had nonzero scores on the MFSAF-TSS and were evaluable for a reduction from baseline.
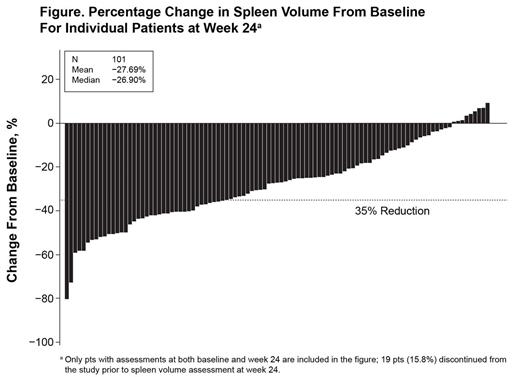
Most pts who had assessments at week 24 (91% [92/101]) had a reduction from baseline in spleen volume (Figure). The study met the primary endpoint, with 31.7% (38/120) of all pts achieving ≥ 35% reduction from baseline at week 24. Overall, 38.3% (46/120) of pts achieved ≥ 35% reduction from baseline in spleen volume at any time on study. As measured by the 7-day MFSAF, 49% (47/96) of pts achieved ≥ 50% reduction from baseline in TSS (median reduction, 47.2%). Pts experienced an improvement from baseline at week 24 in EORTC global health status/QoL (mean change, 5.2).
The most common nonhematologic AEs (≥ 10%) regardless of relationship to study medication included diarrhea (25.8%), upper respiratory tract infection (17.5%), ALT level increased (15.0%), pyrexia (15.0%), AST level increased (13.3%), cough (11.7%), herpes zoster infection (11.7%), nasopharyngitis (10.8%), constipation (10.0%), gamma-glutamyl transferase level increased (10.0%), and headache (10.0%), and most were grade 1/2. Serious AEs were reported for 24.2% of pts, and 65.8% of all pts had grade 3/4 AEs. The most common new or worsening laboratory abnormalities were low hemoglobin (all grade 3, 55.7%), low lymphocyte (grade 3/4, 19.5%), low platelet (grade 3/4, 15.3%), and low ANC (grade 3/4, 7.6%) levels. AEs observed in this study were consistent with those observed in the 2 large phase 3 COMFORT studies. Six pts (5%) died on treatment or within 30 days of discontinuation.
Findings from this study demonstrated that ruxolitinib was relatively well tolerated in Asian pts with MF and provided substantial reductions in splenomegaly and modest improvements in MF-associated symptoms. The AEs observed with ruxolitinib treatment in this study are consistent with those observed in the large phase 3 COMFORT studies, and there were no new AEs associated with ruxolitinib in Asian pts with MF.
Okamoto:Novartis: Honoraria, Research Funding. Sirulnik:Novartis: Employment. Ruiz:Novartis: Employment. Amagasaki:Novartis: Employment. Ito:Novartis: Employment. Akashi:Novartis: Membership on an entity’s Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal