Abstract
A platelet count ≤100,000/µL is regarded as an independent prognostic marker for the development of leukemia and is associated with inferior survival in myelofibrosis (MF) (Huang et al. 2008). The approved JAK2 inhibitor, ruxolitinib, is associated with treatment-emergent thrombocytopenia, and patients with platelets ≤100,000/µL were excluded from the phase III COMFORT trials. Efficacy and safety data are limited in patients with MF and platelets ≤100,000/µL treated with ruxolitinib. Pacritinib (SB1518), an oral JAK2/FLT3 inhibitor, did not appear to be associated with clinically significant treatment emergent anemia or thrombocytopenia during early phase studies in patients with myeloid and lymphoid malignancies. This integrated analysis was performed to further evaluate the safety and efficacy of pacritinib in MF patients with baseline platelet counts of ≤100,000/µL.
The databases from 2 phase I/II clinical trials of pacritinib in advanced myeloid malignancies and MF were integrated to evaluate the rate of adverse events (AEs) and favorable spleen responses in patients with MF and thrombocytopenia.
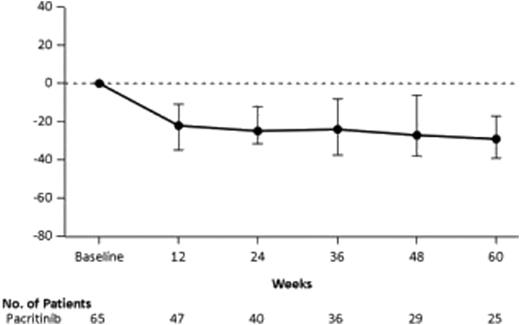
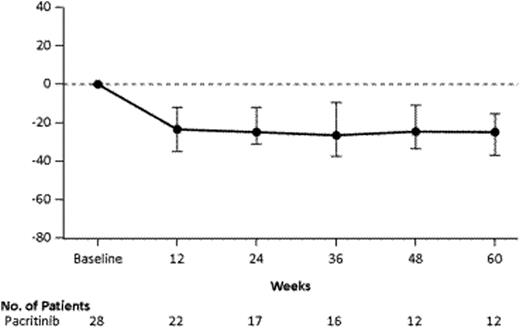
One hundred twenty-nine patients with advanced myeloid malignancies and MF were treated with pacritinib in phase I and II clinical trials. Sixty-five patients with MF were treated with 400 mg orally once daily in 2 phase II studies. Of these, 28 patients with MF [21 primary MF (75%), 5 post-polycythemia vera-MF, 2 post-essential thrombocytosis-MF] had baseline platelet counts of ≤100,000/µL (median: 58,500/µL, range: 15,000/µL – 97,000/µL). The median age was 69 years. Twenty three (82%) patients had the JAK2V617F mutation. During the phase 2 studies, spleen volume responses were assessed by MRI and are shown for all patients (Figure 1) and for patients with platelets ≤100,000/µL (Figure 2). Thirty-seven percent and 43% of all evaluable patients and patients with ≤100,000/µL platelets, respectively, had ≥35% reduction in spleen volume from baseline (Table). Among the 21 informative patients with allelic JAK2V617F quantification at more than 1 study visit, 3, including 2 patients with homozygous mutations, had ≥35% reduction in spleen volume and substantial reductions in allelic burden from baseline (mean reduction 64%, range 44 to 88%). In the 11 (17%) patients with MF and baseline platelet counts ≤50,000/μL, overall spleen volume reduction was 38% (3/8) in evaluable patients and the median decline in platelet count observed at study end was 6,000/µL. Integrated safety analysis for all 129 patients with advanced myeloid malignancies showed the most common adverse events (AEs) were gastrointestinal (GI), predominantly diarrhea, and most of these were grade 1 (43%) and grade 2 (26%). The time to onset of diarrhea was ≤30 days in the majority of those affected, but only 2% had drug discontinuation as a consequence. Among the 129 patients in the phase 1 and 2 trials, 57 patients had ≤100,000 platelets; of these 26 (46%) had no CTC grade change in hemoglobin (Hb) and platelet counts from baseline values. Hb and platelet counts improved by one grade in 16% and 18% of patients, respectively. One grade worsening was seen in 28% and 30% in Hb and platelet counts, respectively.
≥35% REDUCTION IN SPLEEN VOLUME FROM BASELINE BY MRI (EVALUABLE POPULATION with MF)
≥35% REDUCTION IN SPLEEN VOLUME FROM BASELINE BY MRI (EVALUABLE POPULATION with MF)
≥35% REDUCTION IN SPLEEN VOLUME FROM BASELINE BY MRI (EVALUABLE POPULATION with MF)
| STUDY . | N . | At or Before 24 Weeks . | At or Before 36 Weeks . | OVERALL . |
|---|---|---|---|---|
| All Patients | 65 | 13 / 49 (27%) | 17 / 49 (35%) | 18 / 49 (37%) |
| Patients with Platelets ≤100,000/µL | 28 | 7 / 23 (30%) | 10 / 23 (43%) | 10 / 23 (43%) |
| STUDY . | N . | At or Before 24 Weeks . | At or Before 36 Weeks . | OVERALL . |
|---|---|---|---|---|
| All Patients | 65 | 13 / 49 (27%) | 17 / 49 (35%) | 18 / 49 (37%) |
| Patients with Platelets ≤100,000/µL | 28 | 7 / 23 (30%) | 10 / 23 (43%) | 10 / 23 (43%) |
Pacritinib was well-tolerated in patients with MF, regardless of their baseline platelet counts. Grade 1 or 2 GI toxicities, particularly diarrhea, were the most common AEs. Spleen responses were similar in patients regardless of baseline platelet counts (≥100,000/µL vs. ≤100,000/µL). Notably, even patients with initial platelet counts ≤50,000/µL tolerated therapy and the majority maintained stable hemoglobin and platelet counts. A phase III trial will evaluate pacritinib versus best available therapies in patients with MF and platelet counts ≤100,000/µL.
Dean:Cell Therapeutics, Inc: Employment. Cernohous:Cell Therapeutics, Inc: Employment. Mesa:Incyte, CTI, Gilead, Celgene, Genetech, NS Pharma, Lilly: Research Funding. Campbell:Cell Therapeutics, Inc: Employment. Caldwell:Cell Therapeutics, Inc: Employment. Wang:Cell Therapeutics, Inc.: Employment. Myint:Cell Therapeutics, Inc: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal