Abstract
Eltrombopag is an oral thrombopoietin receptor agonist which increases platelet counts in immune thrombocytopenia (ITP) patients by increasing proliferation of megakaryocyte (Mk) precursors and Mk. Maximal approved eltrombopag dosage in chronic ITP patients is 75mg daily, yet some patients do not respond at this dose. In a prior 6-week study, a numerically higher proportion of patients responded at 75mg vs. 50mg. Data of the pharmacokinetics, safety and tolerability of eltrombopag in healthy volunteers at an escalated dosage (100-200mg) showed a dose dependent platelet response. Doses > 75mg have been used in other settings without additional toxicity, including Aplastic Anemia and Chronic Hepatitis C associated thrombocytopenia. Taken in conjunction, a higher eltrombopag dose may be effective in treating ITP in non-responders without increased toxicity. The following double blind, randomized controlled study is in progress to determine if eltrombopag administered at up to 150mg daily increases platelet counts and lessens bleeding symptoms in ITP patients who failed to respond to 75 mg.
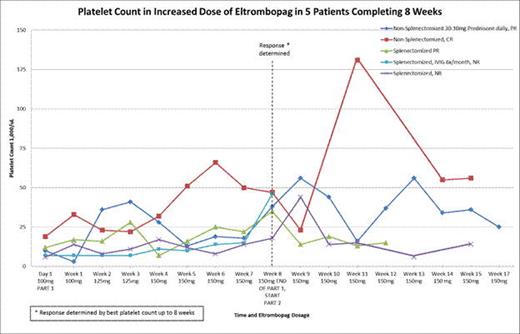
Non-responders (patients ≥ 12 years old with platelet counts<50,000 μL despite 3 weeks of 75mg of eltrombopag daily), stratified by splenectomy status, were enrolled into a double blind randomized controlled study. Patients were allowed to continue stable doses of concomitant medications at randomization. In Part 1 (blinded phase), all patients received 75 mg of eltrombopag with the addition of 25 mg of study drug (eltrombopag or placebo). Every two weeks, doses were increased in 25 mg increments to a maximum daily dose of 150mg. After 8 weeks subjects were unblinded. If on active drug, they can enter the open label (Part 2) phase; or if previously on placebo, subjects may receive open label eltrombopag as per the study protocol to a maximal daily dose of 150mg. Subjects are considered complete responders (CR) with 2 consecutive platelet counts >50,000 μL AND an overall increase from baseline >20,000 μL not attributable to rescue therapy in the 8 weeks from initiating dose escalation. Subjects are considered partial responders (PR) if they have 2 consecutive platelet counts of >50,000 μL OR an overall increase from baseline >20,000 μL not attributable to rescue therapy by 8 weeks (figure). Monitoring includes baseline cataract exams with additional eye exams at 6 and 18 months, bleeding evaluations every 2 weeks (Part 1) and bone marrow biopsy after 1 year (Part 2).
13 patients (2 adolescents and 11 adults) have been enrolled in the study. Of the 5 adult patients who completed ≥ 8 weeks on active medication, 3 achieved either CR (1) or PR (2). The 2 PRs had an increase from baseline to highest count ranging from 23-47,000 μL. 2/3 responders achieved higher platelet counts in the open label extension phase suggesting a longer term slow onset effect of eltrombopag. One PR decreased her daily prednisone dose from 30 mg to 10 mg, with platelet count fluctuations attributed to dietary guideline non-adherence. As of August 8, 6 patients are in Part 1, 4 patients are in Part 2, and 3 have been removed from the study (one patient had elevated transaminases in Part 2, week 12; one patient had pre-existing reticulin fibrosis 2-3+ without clinical symptoms. This pre-study bone marrow result was not available at randomization, but the patient was withdrawn prior to any study drug administration. She had previously received treatment with two other TPO agents; the third patient withdrew secondary to increased bleeding symptoms while on the placebo arm). Other adverse events related to eltrombopag have been mild or moderate. Rescue therapies include intravenous immunoglobulin (IVIG) and prednisone. Most patients have had pre-treatment or recent bone marrows biopsies with a follow up biopsy planned after one year of treatment at 150mg.
To date, the results demonstrate moderate responses to eltrombopag at increased doses to 150mg daily in the 3 responding patients who have been treated the longest. One subject achieved a CR and two a PR. Three subjects were removed for toxicity but in one it was for marrow findings that antedated study enrollment and another for bleeding while receiving placebo therapy. Interim analysis will be performed after 20 enrolled patients and younger patients might enter the study following completion of ongoing eltrombopag studies in pediatric patients with chronic ITP.
Bussel:Ligand: Membership on an entity’s Board of Directors or advisory committees, Research Funding; Shionogi: Membership on an entity’s Board of Directors or advisory committees, Research Funding; Sysmex: Research Funding; Eisai: Membership on an entity’s Board of Directors or advisory committees, Research Funding; Immunomedics: Research Funding; IgG of America: Research Funding; Genzyme: Research Funding; Cangene: Research Funding; GlaxoSmithKline: Equity Ownership, Membership on an entity’s Board of Directors or advisory committees, Research Funding; Amgen: Equity Ownership, Membership on an entity’s Board of Directors or advisory committees, Research Funding; Symphogen: Membership on an entity’s Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal