Abstract
In the absence of a fully matched donor, adult patients with Acute Leukemia (AML and ALL) in CR are nowadays usually offered, as a first choice, an allogeneic transplant from an alternative donor (haplomismatch donor or cord blood cells), but there has been thus far no demonstration that outcome when using an alternative donor is superior to outcome following an autologous stem cell transplantation (ASCT).
We reported last year on a matched pair analysis comparing 113 AML patients transplanted in CR1 with an haplo-mismatch family donor to 226 autologous stem cell transplantations done in the period from January 2000 to December 2010 ( Blood 2013, 3093a). Improvements in both transplant approaches may have changed the outcome, justifying a new analysis.
In the present study, we considered the more recent period from January 2007 to December 2011 and we collected information on patients with AML and ALL transplanted in first (CR1) and second CR (CR2). Also, we considered only T repleted haplo mismatch transplants. During this period a total of 193 fully documented haplomismatch and 2252 ASCT were reported to the EBMT registry.
We used patient age, diagnosis, status at transplant and interval from diagnosis to transplant (< > 6 months for CR1; < > 18 months for CR2) as matching factors. Collection of data on cytogenetics and molecular biology is still in progress.
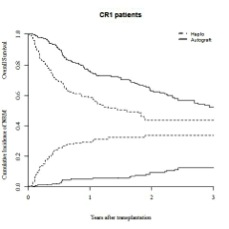
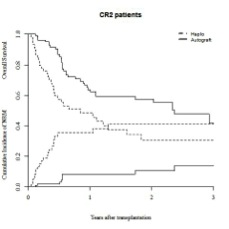
The pair match analysis was done on 184 haplo versus 359 ASCT. The median follow up was 13 months (range, 2-66) for haplo and 14 months (1-72) for ASCT(p=0.9). Patients allografted were transplanted more recently (median year of transplant : 2010 vs 2009, p<10e-4), and they received more frequently total body irradiation in the pretransplant regimen (34% vs 18%; p< 10-4). 5% of the patients in the group haplo received a second allograft, while in the ASCT group 19% of the patients received a subsequent allogeneic transplant and 4% a second autograft.The outcome at two years is presented in the table below:
Following an haplo mismatch transplantation :
- The percentage of acute GVHD grade II+ was 33%
- the incidence of chronic GVHD and extensive GVHD were respectively: 32+/- 3 and 14+/-3%.
By Cox regression analysis introducing age, year of transplantation, diagnosis, status at transplant, TBI in conditioning and the nature of the transplant, ASCT was associated with a better LFS (p=0.05, HR=0.76, 95%CI: .58-.99) and OS (p =10-4 , HR=.53, 95% CI: .40 -.72) than haplomismatch transplant, and a lower non relapse mortality (p< 10-4 ; HR = .27, 95% CI: .17 - .44).
Though this study did not account for cytogenetics and molecular markers (data collection is ongoing), these results suggest that the outcome following ASCT may be better compared to the outcome following a haplo-mismatch transplantation and at least is not inferior. We feel this study support a randomized controlled trial comparing the two transplant modalities in a specific patient population with Acute Leukemia to be defined.
No relevant conflicts of interest to declare.
| 2 year outcome . | . | OS . | LFS . | RI . | NRM . |
|---|---|---|---|---|---|
| all patients | haplo | 44+/-5 | 35+/-4 | 31+/-4 | 34+/-3 |
| auto | 62+/-3 | 47+/-3 | 44+/-3 | 9+/-2 | |
| <0,0001 | 0,02 | 0,0004 | <0,0001 | ||
| CR1 patients | haplo (125) | 49+/-5 | 40+/-5 | 29+/-5 | 30+/-4 |
| auto (250) | 65+/-4 | 50+/-4 | 41+/-4 | 9+/-2 | |
| 0,002 | 0,13 | 0,005 | <0,0001 | ||
| CR2 patients | haplo (59) | 31+/-7 | 24+/-7 | 35+/-8 | 41+/-7 |
| auto (109) | 57+/-6 | 39+/-6 | 49+/-6 | 10+/-4 | |
| 0,003 | 0,09 | 0,04 | <0,0001 |
| 2 year outcome . | . | OS . | LFS . | RI . | NRM . |
|---|---|---|---|---|---|
| all patients | haplo | 44+/-5 | 35+/-4 | 31+/-4 | 34+/-3 |
| auto | 62+/-3 | 47+/-3 | 44+/-3 | 9+/-2 | |
| <0,0001 | 0,02 | 0,0004 | <0,0001 | ||
| CR1 patients | haplo (125) | 49+/-5 | 40+/-5 | 29+/-5 | 30+/-4 |
| auto (250) | 65+/-4 | 50+/-4 | 41+/-4 | 9+/-2 | |
| 0,002 | 0,13 | 0,005 | <0,0001 | ||
| CR2 patients | haplo (59) | 31+/-7 | 24+/-7 | 35+/-8 | 41+/-7 |
| auto (109) | 57+/-6 | 39+/-6 | 49+/-6 | 10+/-4 | |
| 0,003 | 0,09 | 0,04 | <0,0001 |
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal