Abstract
Outcome of patients with high-risk acute myeloid leukemia (AML) not undergoing an allogeneic transplant after achieving complete remission (CR) is extremely poor. The risk of disease progression is high and the unavailability of an HLA identical sibling might jeopardizes their outcome, if the time to transplant from a matched unrelated donor (MUD) is expected to be longer than 3 months from CR. Being these patients on urgency to be transplanted, the search for an alternative donor should be preferably addressed towards the cord blood (CB) banks or an haploidentical family donor. Herein, we report the results on unmanipulated, G-CSF primed, haploidentical bone marrow (BM) transplantation in patients with high-risk AML in CR lacking a suitable HLA-identical donor.
from January 2008 to July 2013, 57 patients with a median age of 44 yrs (range, 5-66) (2 children aged 5 and 14 yrs) with very high-risk AML (CR1=32; CR2=14; advanced phase=11) underwent BM transplant from an haploidentical family donor (sibling=23; offspring=21; mother=10; father=3). All patients received a uniform myeloablative (MAC= 42 fit patients <55 yrs) or Reduced Intensity (RIC=15; unfit patients or >55 yrs) conditioning regimen consisting of Thiotepa, i.v.Busulphan and Fludarabine (TBF) combination. All 57 patients received an identical GvHD prophylaxis consisting of pretransplant antithymocyte globulin (ATG) combined with cyclosporine, methotrexate, mycophenolate mofetil and basiliximab, an anti-CD25 monoclonal antibody. Donors were primed with G-CSF at 4 μg/Kg/d for 7 consecutive days. BM was harvested on day 0 and infused unmanipulated.
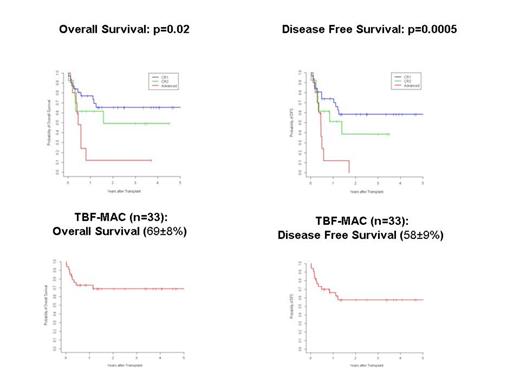
the median number of CD34+ and CD3+ cells infused was 2 (0.6-11)x106/Kg and 3 (0.9-17)x107/Kg, respectively. Two patients died early. All 55 evaluable patients engrafted at a median of 20 days (range,12-29) and the cumulative incidence (CI) of neutrophil engraftment was 96.5±0.1% at 30 days. The 100-day CI of II-IV and III-IV grade acute GVHD was 33±0.4% and 11±0.2%, respectively. Extensive chronic GVHD occurred in 6 out of 51 (12%) evaluable patients and the 2-year CI of extensive chronic GVHD was 18±0.4%. The 6-mos and 1-year CI of transplant-related mortality (TRM) was 24±0.4% and 26±0.4%, respectively. The overall CI of relapse was 20±0.4% at 1-year and 38±0.8% at 5-year. With a median follow-up of 30 mos (range, 4-67), the 5-year probability of overall (OS) and disease-free survival (DFS) was respectively 52±7% and 43±7% for all patients, 65±9% and 58±9% for patients in CR1, 49±15% and 38±16% for patients in CR2, 12±11% and 0.0% (at 3yrs) for patients transplanted in advanced phase. For 33 patients transplanted in early (CR1+CR2) disease stage and conditioned with the TBF-MAC regimen, the 5-year probability of OS and DFS was 69±8% and 58±9%, respectively, while OS and DFS at 3 yrs were 45±15% for 11 patients in early phase receiving the TBF-RIC regimen.
Haploidentical transplant using G-CSF primed, unmanipulated BM is correlated with high engraftment rate, low incidence of acute and chronic GVHD, acceptable TRM and favorable outcome. This approach represents a valid and feasible alternative to MUD or CB transplant for high-risk AML patients in complete remission and on urgency to be transplanted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal