Abstract
In a phase I/II trial of a novel bortezomib-based regimen for reduced-intensity conditioning (RIC) hematopoietic stem cell transplantation (HSCT) recipients of HLA-mismatched peripheral blood stem cell (PBSC) grafts, we documented low rates of graft-versus-host disease (GVHD) and non-relapse mortality (NRM), with promising survival. In registry analyses, myeloablative conditioning (MAC) HSCT recipients of both HLA-matched (MUD) and 1-locus mismatched donor (MMUD) grafts also have impaired outcomes, with day +100 grade III-IV acute GVHD rates of 28% and 37% respectively, 1-year NRM of 36% and 45% respectively, 1-year progression-free (PFS) of 47% and 38% respectively, and 1-year overall survival (OS) of 52% and 43% respectively. We therefore evaluated a similar bortezomib-based regimen in MAC HSCT recipients lacking 8/8 HLA-matched (-A, -B, -C, -DRB1) related donors.
In a prospective single-arm phase II trial, we enrolled patients with hematologic malignancies, aged 18-60 years, receiving MUD, MMUD, or mismatched related donor (MMRD) grafts. Myeloablative conditioning was IV busulfan (130 mg/m2, without PK dose adjustment) and fludarabine (40 mg/m2) once daily for 4 doses (days -7 to -4). T-replete PBSC grafts with ≥ 2x106 CD34+ cells/kg were infused on day 0. GVHD prophylaxis comprised bortezomib (1.3 mg/m2 IV on days +1, +4, +7), methotrexate (15 mg/m2 IV on day +1, 10 mg/m2 on days +3, +6, +11) and tacrolimus from day -3, with a planned taper starting day +100 and complete by day +180. The primary endpoint was day +100 acute GVHD incidence. Secondary endpoints included NRM, relapse, PFS, OS and chronic GVHD at 1 year.
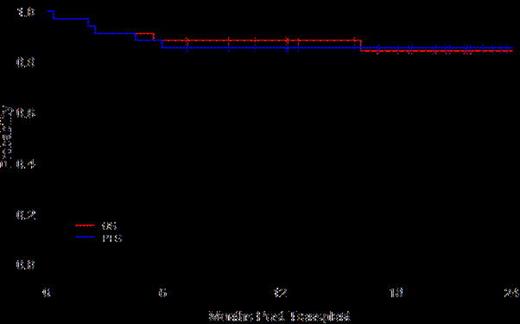
The 34 patients (19 male, 15 female), accrued between March 2011 and November 2012, had a median age of 49 years (range, 21-60) and variable diagnoses (17 AML, 6 MDS, 4 NHL, 3 MPD, 2 ALL, 1 CML, 1 MM) and disease risk indices (Low 1, Intermediate 24, High 9). They received 8/8 MUD (n=14), 7/8 MMUD (n=18) or 7/8 MMRD (n=2) PBSC grafts. Mismatches (16 antigen-, 4 allele-level) involved HLA-A (9), -B (1), -C (6) and -DRB1 (4). The median follow up in survivors is 20 months (range, 7.2-25.5).
In conclusion, bortezomib-based prophylaxis for MAC HSCT recipients of HLA-mismatched and unrelated donor grafts was safe and well-tolerated, with low rates of severe acute GVHD, NRM and relapse, and excellent long-term survival. On preliminary landmark analysis, upper GI GVHD did not appear to impair transplantation outcomes. Bortezomib-based prophylaxis is suitable for prospective randomized evaluation in myeloablative transplantation recipients lacking HLA-matched related donors.
Koreth:Millennium pharmaceuticals: Research Funding; Takeda Pharmaceuticals: Consultancy. Off Label Use: Bortezomib for GVHD prophylaxis.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal