Abstract
BRONJ is a complex process that involves interplay of drug effect, bacteria-host immune interactions, and alteration of cytokines and inflammatory mediators leading to impaired healing of the mucosa. In this prospective study, we evaluated MM patients on long term BP therapy to define risk factors and explore cytokine changes in relationship to BP infusion and development of BRONJ.
110 MM patients were enrolled on the study and followed for 18 months. Patients were receiving zoledronic acid infusions once a month (n=75) or every 3 months (n=35) for those in stable remission > 3 years. Patients had clinical and oral evaluations at each visit. Blood samples were collected at baseline and every 6 months. Saliva samples were obtained every 3 months (before and 15 minutes after zoledronic acid infusions). Cytokine expression was analyzed using MULLIPLEX MAP Multiplex Assay (EMD Millipore, MA).
Median time from MM diagnosis was 3.7 years (range: 2.5-13) for 100 patients; 10 newly diagnosed patients had a median of 7 months (range: 1-9). Median age was 57 years (range: 33-81); 58 were Caucasians, 49 African American, 3 Asians; 68 were males. At study entry, 87 (79%) patients were in remission: CR (n=35, 32%) of them 15 were in CR for > 7 years, PR (n=52, 47%) and PD (n=23, 21%). At study entry, 24 patients were not receiving any MM therapy; most were on maintenance with lenalidomide (n=59), and 10 were receiving induction. While on study, 50 patients progressed and received salvage therapies that included: bortezomib based (n=14), lenalidomide (n=6), carfilzomib (n=16) and other clinical trials (n=14). Thirteen patients died: 9 from complications of relapsed MM and 4 from other causes. Eighteen patients withdrew consent for sample collection and dental evaluations but were followed clinically. Most patients had history of dental procedures (extractions, n=80). The predominant pathology detected during dental evaluations included: moderate/severe periodontal disease (n=45) and gross dental caries (n=15); while on the study, 66 patients continued regular dental cleaning and 10 had dental extractions. During the 18 months of follow up, 14 patients developed new lesions with exposed bone for 8 weeks, meeting the definition of BRONJ. Median time from MM diagnosis to BRONJ was 5.7 years (the 95% CI: 1.9-12.0). BRONJ patients were in remission (n=9), receiving monthly zoledronic acid (n=9), dental extractions (n=9) and three had recurrent BRONJ. There was no association found between BRONJ and diabetes, smoking, or dental pathology. BRONJ treatment was conservative consisting of antibiotics and holding BP therapy. There are 5 patients who continue to have non-healing BRONJ lesions.
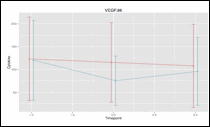
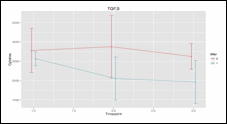
Saliva and serum samples obtained during this study (baseline, midpoint (6-9 months), end (12-18 months) were assessed for the following cytokines: interleukins (IL)-1β, -6, and -17; TNF-α, IFN-α, TGF-β, MIP-1 α β, MMP-9, Osteopontin, Osteocalcin, RANKL, Osteoprotregerin, VEGF and EGF in 43 patients with ONJ (n=13) and without ONJ (n=30). There were statistically significant lower levels of VEGF and TGF- β (p= .04 and .02, respectively) in the serum overtime in patients who developed BRONJ, figure below. In the saliva cytokines levels were significantly lower in patients who developed BRONJ vs no BRONJ at baseline, before and after zoledronic acid infusions: [Mean pg/ml (SD), p value]: MIP-1 β [14 (3) vs 6(2), p=0.01]; IL-1 β [1824 (1518) vs 72 (38), p=0.04]; IL-6 [15 (4) vs 3 (3), p=0.02]; TNF-α [10 (3) vs 3 (2), p=0.09]. Osteoprotregerin [213 (39) vs 125 (26), p=0.07] was borderline higher in those without BRONJ.
Figure: VEGF and TGF- β in serum of MM patients with BRONJ (n=13) vs no BRONJ (n=30)
Figure: VEGF and TGF- β in serum of MM patients with BRONJ (n=13) vs no BRONJ (n=30)
the incidence of BRONJ remains high at 12% after a median of 5 years of BP use. Dental extraction remains the most significant risk factor for BRONJ. The salivary cytokine repertoire suggests M1 macrophage polarization (recently reported by Zhang et, Clin Cancer Res 2013), in response to injury. The low levels of VEGF and TGF in the serum in response to injury further impair the mucosal healing.
1. Baseline, 2. Midpoint (6-9 months), 3. End of study (12-18 months)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal