Abstract
Acute myeloid leukemia (AML) remains the most common form of acute leukemia in adults but the treatments, in the past several decades, have not led to satisfactory results. Serious infections and therapy resistance or relapsed are the main causes of mortality among these patients.
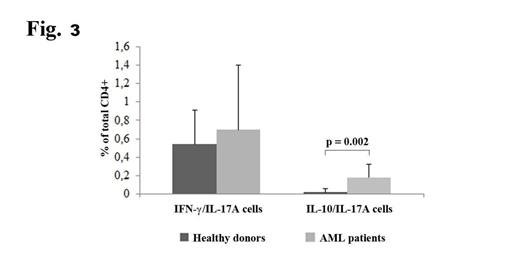
IL-17 producing helper T cells (Th17) play in humans, pleiotropic roles in protection against a range of predominantly extracellular bacterial and fungal pathogens, in the pathogenesis of many inflammatory and autoimmune diseases and a controversial role in protection or progression of tumors. In particular, recently has been demonstrated a remarkable plasticity of these cells to transdifferentiate, depending of the stimuli, in a Th1-like Th17 cells (secreting IFNg with tumor suppressor activity) or in a Treg-like Th17 cells (secreting IL-10 with tumor promoter activity). Moreover, few reports indicate that the number of Th17 in patients with hematological malignancies was increased in peripheral blood, however their role and their relationship with respect to other T helper cells, particularly in AML, have not yet been clarified.
Our study aims to investigate the role of T helper cells in AML, with particular focus to Th17 cells, hypothesizing their contribution in severe infections developed by these patients and in the high rate of recurrence of the disease.
Samples of peripheral blood were collected from 20 newly diagnosed AML patients of any FAB (except promyelocitic) before any treatment and 20 sex and age-matched healthy volunteers. Mononuclear cells (PBMCs) were separated by density gradient centrifugation.
Intracellular IFN-γ, IL-17A and IL-4 expression was performed using the human Th1/Th2/Th17 phenotyping kit after stimulation of CD4+ cells with IL-6 (25 μg/ml), phorbol 12-myristate-13-acetate (50 ng/ml) and ionomycin (1 μg/ml).
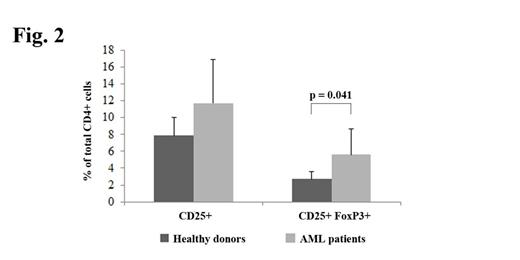
For Tregs analysis, PBMCs were stained with anti-human FITC CD4, APC-Cy7 CD25 and APC Foxp3 and analyzed using a FACSCanto flow cytometer.
For the analysis of cytokine secretion, human IL-17 and IL-10 secretion - detection kits were used.
This finding, if confirmed, could suggest new therapeutic strategies more oriented towards immunomodulation rather than cytoreduction.
Martinelli:NOVARTIS, BMS(Consultancy and speaker bureau), PFIZER, ARIAD (Consultancy): Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal