Abstract
aHUS is a rare, genetic, life-threatening disease of uncontrolled, chronic complement activation leading to TMA and severe end-organ damage. During the first clinical manifestation, end-stage renal disease (ESRD) or death occurs in approximately 33 to 40% of patients, and within one year of diagnosis, up to 65% have permanent renal damage, ESRD, or die despite receiving plasma exchanges/plasma infusions (PE/PI). Many aHUS pts are also misdiagnosed as TTP, which also results in poor outcomes with PE/PI. Hence, early diagnosis and effective treatment are critical to halt and/or prevent systemic complement-mediated damage. Ecu, a terminal complement inhibitor, is approved for the treatment of aHUS. Herein, we report safety and efficacy results of Ecu from the largest prospective study in aHUS to date.
This was an open-label, single-arm, Phase 2 trial of Ecu in adult aHUS pts. Inclusion criteria included platelet count <150 x109/L and LDH ≥1.5 ULN. Pts with STEC-HUS (shiga toxin + E. coli) and severe ADAMTS13 deficiency (<5%) were excluded. An identified complement gene mutation was not required for admission. The primary endpoint was complete TMA response at 26 wks (normalization of platelets and LDH, and ≥25% improvement in serum creatinine from baseline (BL) on 2 consecutive measurements ≥4 wks apart).
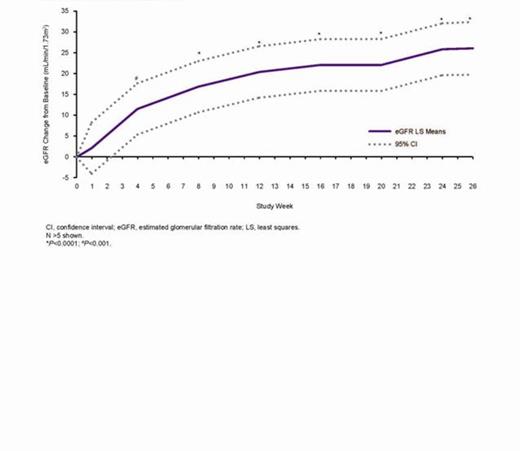
41 pts enrolled and 38 (93%) received 26 wks of treatment (Table). 30 pts (73%) were newly diagnosed, with a median of 2 wks to the first dose of Ecu. 6 pts (15%) had no PE/PI during the current clinical manifestation. At wk 26, 30 pts (73%) achieved complete TMA response, 36 (88%) achieved hematologic normalization, and 40 (98%) achieved platelet count normalization. Mean increase in platelet count from BL was 119x109/L (P<0.0001). Mean eGFR increase from BL was 26.1 mL/min/1.73 m2 (P<0.0001). Platelet count (Fig 1) and eGFR (Fig 2) increased significantly from BL through wk 26. Of 24 pts on dialysis at BL, 20 (83%) discontinued dialysis by wk 26. Two pts not on dialysis at BL initiated and remained on dialysis through 26 wks. QoL significantly improved. Ecu was generally safe and well tolerated. Two pts had meningococcal infections, one of whom continued Ecu. No pts died.
Baseline characteristics
| Baseline Demographics and Disease Characteristics (N=41) . | |
|---|---|
| Age, mean (SD), y | 40.3 (15.3) |
| Female sex, n (%) | 28 (68) |
| Identified complement regulatory protein mutation or auto-antibody, n (%) | 20 (49) |
| Time from aHUS diagnosis until screening (mo), median (range) | 0.8 (0–311) |
| Newly diagnosed pts, n (%) | 30 (73) |
| Duration of current clinical manifestation of aHUS (mo), median (range) | 0.5 (0.0–19.1) |
| PE/PI during current clinical manifestation of aHUS, n (%) | 35 (85) |
| Dialysis at BL, n (%) | 24 (59) |
| Prior renal transplant, n (%) | 9 (22) |
| Plt count <150x109/L, n (%) | 27 (66) |
| LDH >ULN, n (%) | 32 (78) |
| eGFR ≤60 mL/min/1.73 m2, n (%) | 41 (100) |
| Efficacy Outcomes | |
| Complete TMA response*, n (%) | 30 (73) |
| Hematologic normalization†, n (%) | 36 (88) |
| Plt count normalization‡, n (%) | 40 (98) |
| Plt count increase (x109/L), mean (95% CI) | 119 (94; 145) P<0.0001 |
| eGFR increase from BL ≥15 mL/min/1.73 m2,n (%) | 22 (54) |
| eGFR increase from BL (mL/min/1.73 m2), mean (95% CI) | 26.1 (19.8; 32.4) P<0.0001 |
| CKD improvement ≥1 stage from BL, n (%) | 26 (63) |
| Baseline Demographics and Disease Characteristics (N=41) . | |
|---|---|
| Age, mean (SD), y | 40.3 (15.3) |
| Female sex, n (%) | 28 (68) |
| Identified complement regulatory protein mutation or auto-antibody, n (%) | 20 (49) |
| Time from aHUS diagnosis until screening (mo), median (range) | 0.8 (0–311) |
| Newly diagnosed pts, n (%) | 30 (73) |
| Duration of current clinical manifestation of aHUS (mo), median (range) | 0.5 (0.0–19.1) |
| PE/PI during current clinical manifestation of aHUS, n (%) | 35 (85) |
| Dialysis at BL, n (%) | 24 (59) |
| Prior renal transplant, n (%) | 9 (22) |
| Plt count <150x109/L, n (%) | 27 (66) |
| LDH >ULN, n (%) | 32 (78) |
| eGFR ≤60 mL/min/1.73 m2, n (%) | 41 (100) |
| Efficacy Outcomes | |
| Complete TMA response*, n (%) | 30 (73) |
| Hematologic normalization†, n (%) | 36 (88) |
| Plt count normalization‡, n (%) | 40 (98) |
| Plt count increase (x109/L), mean (95% CI) | 119 (94; 145) P<0.0001 |
| eGFR increase from BL ≥15 mL/min/1.73 m2,n (%) | 22 (54) |
| eGFR increase from BL (mL/min/1.73 m2), mean (95% CI) | 26.1 (19.8; 32.4) P<0.0001 |
| CKD improvement ≥1 stage from BL, n (%) | 26 (63) |
Complete TMA response: normalization of plts and LDH, and ≥25% improvement in serum creatinine from BL on 2 consecutive measurements ≥4 wk apart.
Complete hematologic response: plt and LDH normalization at ≥2 consecutive measurements ≥4 wk apart.
Plt count normalization: plt count ≥150x109/L ≥2 consecutive measurements ≥4 wk apart.
Platelet count improvement through 26 weeks.
eGFR improvement through 26 weeks.
Ecu normalized hematologic parameters and significantly improved renal function and QoL. The results of this prospective study confirm that Ecu inhibits complement-mediated TMA in adult aHUS pts, and point to the importance of early and accurate diagnosis, including ADAMTS13 testing. Due to high morbidity and mortality in aHUS despite PE/PI, recent guidelines recommend Ecu as first-line treatment in adults once an unequivocal diagnosis is made. The current data validate this treatment approach. This study is ongoing.
Weekers:Roche, Novartis, Astellas: Grant Support Other, Research Funding. Ogawa:Alexion Pharmaceuticals: Employment. Bedrosian:Alexion Pharmaceuticals: Employment.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal