Abstract
Haploidentical stem cell transplant (haplo-HCT) is a therapeutic option for patients without matched donors. We aimed to analyze outcomes of patients with AML/MDS treated with melphalan-based conditioning and different donors at our institution and determine the factors associated with survival.
All 246 patients receiving an allograft for AML/MDS between 01/2005 and 09/2012 were included in this retrospective analysis. Conditioning regimen consisted of melphalan 100 mg/m2 (Mel100) (N=37) or 140 mg/m2, (Mel140) (N=209) and fludarabine 120-240 mg/m2 +/- thiotepa (N=50). Graft versus host disease (GvHD) prophylaxis had consisted of tacrolimus and mini-methotrexate +/- ATG for matched transplants, and post-transplant cyclophosphamide (PTCy), tacrolimus and mycophenolate mofetil (MMF) for T-cell replete (TCR) haploidentical transplants. A small number of patients (N=19) received a T-cell depleted (TCD) haplo-HCT using CD34+ selected graft as previously described by us. We analyzed transplant outcomes and performed lymphocyte reconstitution on available samples from MRD, MUD and TCR-haplo recipients between day+30 and +365 post-transplant. Incidences in GvHD were assessed using Fisher's exact test. Differences in CD3+ T-cell counts were assessed using Kruskal-Wallis test. Kaplan-Meier survival curves were used to estimate OS, and PFS and the log-rank test was used to assess differences between groups; NRM was determined by the cumulative incidence (CI) function using the competing risks method. The competing risk included was relapse. Differences in cumulative incidence NRM between groups were assessed using Gray's test.
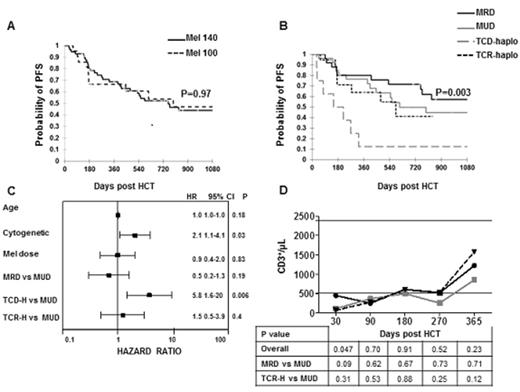
Median follow-up for survivors was 31 months. PFS for the entire cohort at 1 year was 44% and OS was 53%. No differences in outcomes (NRM, relapse, PFS) were noted for patients treated with ablative (140 mg/m2) or reduced dose (100mg/m2) of melphalan, both overall and for patients in remission(Fig.1A). To appreciate the impact of different donor type of transplant outcomes we analyzed outcomes of patients treated in remission (CR1+CR2) (N=78). Pre-transplant characteristics were well balanced for patients who received a MSD, MUD or haplo donor except TCR haplo patients received almost exclusively a bone marrow graft (95%) and TCD-haplo patients had a younger median age at transplant (27.5 years; P=0.0004). For patients in remission at transplant, 1 year PFS was 67% (Mel100) vs. 69% (Mel140) (P=0.97). Based on donor type, the 1-year PFS were 80% for MRD (N=25) recipients, 76% for MUD (N=26) recipients, 64% for TCR haplo (N=19) and only 13% for TCD-haplo recipients (N=8) (P=0.003) (Fig.1B).
(A) PFS by Mel dose for patients in CR1+CR2; (B) PFS by donor type for patients in CR1+CR2. (C) Multivariable analysis for PFS in CR1+CR2 patients (D) CD3 immune-reconstitution for MRD, MUD and TCR-haplos (medians).
(A) PFS by Mel dose for patients in CR1+CR2; (B) PFS by donor type for patients in CR1+CR2. (C) Multivariable analysis for PFS in CR1+CR2 patients (D) CD3 immune-reconstitution for MRD, MUD and TCR-haplos (medians).
In univariate and multivariable analyses for PFS, the only significant factors associated with worse survival were cytogenetic risk category and the use of a TCD haplo-HCT (Fig.1C). Using MUD donor as reference, no differences were detected in PFS when compared with recipients of MRD or TCR-haplodonors, while TCD-haplo group did significantly worse (multivariable analysis; P=0.006).
The CI NRM rates for CR1+CR2 patients at 100 days were 0% (MRD), 5% (TCR-haplo), 4% (MUD), 38% (TCD-haplo), and at one year were 8% (MRD), 18% (TCR-haplo), 8% (MUD), and 75% (TCD-haplo) (P=0.0008).
Incidence of severe aGvHD was 0% (TCR-haplo), 4% (MUD, MRD), and 50% (TCD-haplo) (P=0.0008). Overall chronic GvHD incidence was lowest in the TCR-haplo group (16%) and highest in the MRD group (48%). TCD-haplo and MUD had cGvHD rates of 25% and 34%, respectively (P=0.16).
As shown in Fig.1D, TCR-haplo recipients reconstituted lymphocyte subsets with a kinetic trend similar to MUD and MRD recipients. All patients achieved normal CD3+ T-cell counts around day 180 post-transplant, with an early recovery of CD8+ T cells. TCR-haplo recipients did not have a significant inferior reconstitution for CD4+, CD8+, CD3-CD56+ and CD3-CD20+ cells at any time point between day 90 and day 365.
Outcomes of patients with AML/MDS treated with melphalan-based conditioning are negatively influenced by cytogenetic risk category and the use of a TCDhaplo donor, while melphalan dose and the use of a TCR haplo-HCT vs. matched donor did not negatively impact survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal