Abstract
Multiple myeloma (MM) is uncommon in patients below 40 years of age. Between 1960 and 1992 when stem cell transplantation (SCT) was rarely performed and novel agents were unavailable, overall survival (OS) was reported to be 54 months in the Mayo Clinic series of patients with MM below forty years of age. The impact of novel agents or SCT in this population is unclear. Herein, we report the outcomes of patients under 40 years of age who were evaluated over a span of more than five decades with a focus on the periods contemporaneous with the introduction of SCT and novel agents, the major therapeutic milestones in the management of MM.
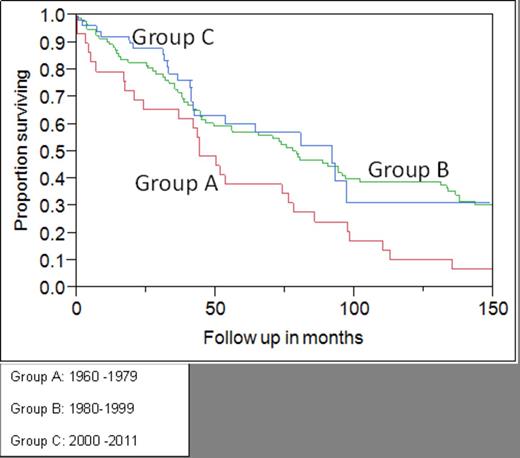
We analyzed the medical records of patients with MM under 40 years of age who were evaluated at Mayo Clinic, Rochester, MN between 1/1/1960 and 12/31/2011. SCT and novel agents were utilized infrequently prior to the years 1990 and 2000, respectively. Patients were therefore divided into three cohorts by the year of diagnosis of MM: Group A (1960 -1979), Group B (1980 to 1999) and Group C (2000 –2011) to assess the impact of major therapeutic advances (i.e. Increased utilization of SCT and novel agents compared to conventional chemotherapy). OS was calculated by the Kaplan -Meier method.
Out of 8063 unique MM patients seen at our institution during this period, 174 (2%) patients were under 40 years of age at diagnosis. The median age at diagnosis was 36 years (range: 19-39). The estimated median follow-up of the entire cohort was 179 months (95% CI: 149-196 months). The median OS of the entire cohort was 76 months (95% CI: 45-80 months) from diagnosis. The median OS of patients in Groups A (n=29, 17%), B (n=93, 53%), and C (n=52, 30% ) was 44 months (95% CI: 20- 76), 79 months (95% CI: 46-97), and 92 months (95% CI: 42-NR), respectively (p=0.005). No significant OS difference was noted between Groups B and C (Figure). Sixty-six (38%) patients underwent at least one SCT (autologous: 56 patients and allogeneic 10 patients). The utilization of SCT increased over the three time periods from Group A 0%, Group B 39% and Group C 58% (p<0.001). Of 153 patients in whom front-line therapy-related data were available 118 (77%) received conventional and 35(23%) received novel agents. The median OS of patients who underwent transplantation (n=66) was 93 months compared to 46 months for those who did not (n=108, p=.01). In the 66 patients who underwent SCT, the median OS was 93 months for conventional agents-based induction (95% CI: 73-143) versus 97 months (95% CI: 41-187) for novel agent based induction (p=.4).
Sixty-eight (40%) patients received novel agents at some point during the course of their disease [bortezomib 35 (54%), thalidomide 44 (67%), lenalidomide 47 (71%) and pomalidomide 7(11%)]. The median survival of these patients was 131 (95% CI: 88-161) months versus to 46 (CI: 37-74) months for those (n=106) receiving conventional agents only (p=0.0002).
OS of patients with MM under 40 years of age in the pre-transplant era (Group A) was significantly shorter than that of patients diagnosed in the era of SCT (Group B) and SCT plus novel agents (Group C). Although improvement of survival outcomes is evident with utilization of novel agents, similar outcomes of Groups B and C indicate lack of incremental benefit over SCT with utilization of novel agents. Maximal survival gain coincides with the introduction of SCT in this unique patient cohort.
Kumar:Celgene: Consultancy, Research Funding; Millennium: Consultancy, Research Funding; Onyx: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal