Abstract
Umbilical cord blood transplantation (UCBT) is often complicated by delayed engraftment and higher rates of engraftment failure. We sought to investigate the outcomes of patients undergoing UCBT2 after engraftment failure compared to those who had autologous hematopoietic recovery and did not receive UCBT2.
We reviewed the medical records of 186 patients who received UCBT between 2001 and 2011 at the Case Comprehensive Cancer Center [Seidman Cancer Center, University Hospitals Case Medical Center and Taussig Cancer Institute, Cleveland Clinic]. Standard definitions of engraftment were used. Patients who died or had progressive disease before day 30 were excluded (n=9), as they were considered inevaluable for engraftment.
Twenty-seven patients (15%) had primary engraftment failure; twelve had autologous hematopoietic recovery and 15 presented no recovery (Table). The median total nucleated cell dose for the first UCBT was 2.56x107 cells/kg (range 1.23 x107 - 5.69x107), not statistically different from patients achieving engraftment (p = 0.29). The cause of engraftment failure could not be identified in 22 patients.
Demographic characteristics and outcomes of patients with primary engraftment failure or autologous hematopoietic recovery after UCBT.
| Median Age (Range) (years) . | 49 (20-65) . | ||
|---|---|---|---|
| Female / Male | 10 / 17 | ||
| Diagnosis | |||
| AML | 13 | ||
| ALL | 3 | ||
| CML | 4 | ||
| NHL | 3 | ||
| PCM | 1 | ||
| MDS | 2 | ||
| Aplastic Anemia | 1 | ||
| UCBT #1 | UCBT #2 | ||
| Conditioning Regimen | |||
| Reduced Intensity | 23 | 15 | |
| Myeloablative | 4 | 0 | |
| Number of Units | UCBT #1 | UCBT #2 | |
| 1 | 10 | 4 | |
| 2 | 14 | 11 | |
| >2 | 3 | 0 | |
| Autologous Hematopoiesis | Second UCBT | p value | |
| Overall Survival (days) | 301 | 273 | ns |
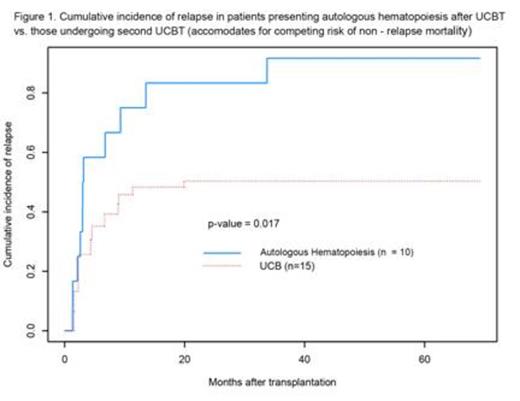
| 40 month cumulative incidence of relapse | 92% | 50% | p = 0.017 |
| Median Age (Range) (years) . | 49 (20-65) . | ||
|---|---|---|---|
| Female / Male | 10 / 17 | ||
| Diagnosis | |||
| AML | 13 | ||
| ALL | 3 | ||
| CML | 4 | ||
| NHL | 3 | ||
| PCM | 1 | ||
| MDS | 2 | ||
| Aplastic Anemia | 1 | ||
| UCBT #1 | UCBT #2 | ||
| Conditioning Regimen | |||
| Reduced Intensity | 23 | 15 | |
| Myeloablative | 4 | 0 | |
| Number of Units | UCBT #1 | UCBT #2 | |
| 1 | 10 | 4 | |
| 2 | 14 | 11 | |
| >2 | 3 | 0 | |
| Autologous Hematopoiesis | Second UCBT | p value | |
| Overall Survival (days) | 301 | 273 | ns |
| 40 month cumulative incidence of relapse | 92% | 50% | p = 0.017 |
Among patients with engraftment failure without autologous recovery, 2 patients did not receive further salvage and died at 40 and 48 days after first UCBT; 2 others received backup autologous hematopoietic cell infusions and 11 received UCBT2. In patients with autologous hematopoietic recovery, 8 did not receive a UCBT2 because disease remission had been attained (n=4), active infection (n=1), relapsed disease beyond 40 days after UCBT (n=1) or absence of compatible donor (n=1).
Fifteen patients (engraftment failure [n=11]); autologous recovery, [n=4]) underwent UCBT2, at a median of 43 days (range 33-244) from first to second UCBT. All patients received non–myeloablative second conditioning regimens. Four patients received one UCB unit and 11 received two units. Neutrophil engraftment after UCBT2 was observed in 10 of 15 patients at a median of 30 days (range, 13-35).
The median survival for the entire cohort was 272 days (range 40–2130); one year overall survival was 36%. Engraftment and overall survival were not statistically different between those receiving 1 or 2 UCB units for UCBT2. Overall survival was not statistically different between patients who underwent UCBT2 and those who had autologous recovery or backup autologous infusions without further salvage.
The proportion of patients in remission was similar in the 2 subgroups (UCBT2, 53%; autologous recovery, 50%). Relapse occurred in 2/15 patients who underwent UCBT2 and 8/10 patients who had autologous recovery or backup infusions. Forty months after transplantation, the cumulative incidence of relapse was 92% after autologous recovery vs. 50% after UCBT2 (Figure). Non–relapse mortality after UCBT2 was 73%.
Engraftment failure after UCBT frequently has no identifiable cause, and is associated with high morbidity and mortality. UCBT2 is feasible and can result in engraftment in the majority of patients, but is limited by patient condition after transplant as well as the availability of compatible grafts. UCBT2 is associated with significantly better disease control than continued autologous hematopoiesis, but additional efforts are necessary to reduce the high risk of non-relapse mortality in this group of patients.
Hill:Celgene: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal