Abstract
The improvements in genetic characterization of AML allowed the ELN to propose a prognostic classification into 4 categories: Favorable, Intermediate I, Intermediate II and Adverse. Several groups have tested the outcome of AML patients based on these genetic subgroups in registries and databases from prospective trials. Since ALLOSCT recommendations are being established based on the ELN risk categories, we considered of interest to investigate whether these also have an impact on the results of allogeneic transplants. This could be helpful to identify the patients that may benefit the most from ALLOHCT in the first complete remission (CR1).
To investigate whether the ELN genetic groups of AML have any impact on the results of ALLOHCT performed in CR1. To identify the patients who are best candidates for transplantation, based on the ELN categories as well as in other characteristics.
Patients were transplanted between 1990 and 2012. In all cases, treatment prior to transplant had consisted of anthracycline based induction and intermediate-dose cytarabine consolidation according to the CETLAM AML-88, AML-94, AML-99 and AML-03 trials. Upper age limit for transplantation was 60 years until 2002 and 70 years thereafter. Most patients above 50 years received either CD34 selected grafts or reduced intensity conditioning. GVHD prophylaxis after transplant was usually based on cyclosporine and prednisone or methotrexate. The main characteristics of patients and transplants were included in the exploratory analysis of variables influencing survival; those with a p- value up to 0.1 were incorporated as covariates to the multivariable model.
One hundred ninety two patients in CR1 received an ALLOHCT from HLA-identical siblings (n=140), adult unrelated donors (n=26) or umbilical cord blood (n= 26). Age distribution of the patients was as follows: 16-35 years-old (y-o) n=65 (34%), 36-50 y-o n= 55 (29%), 51-60 y-o n= 54 (28%), >60 y-o n=18 (9%). Twenty-three patients (12%) were classified as in the favorable ELN category, 54 (28%) in the intermediate I, 41 (21%) in the intermediate II and 74 (39%) in the adverse. One-hundred fifty-seven patients (82%) had achieved CR1 after a single course of chemotherapy. Conditioning was myeloablative (MA) in 139 (72%) patients and reduced-intensity (RIC) in 53 (28%). In 76 cases of the MA regimens total body irradiation was included.
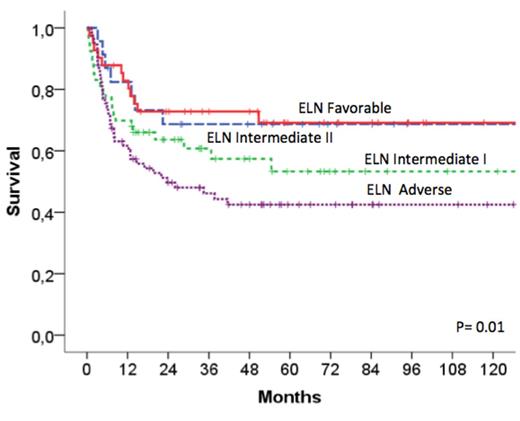
Thirty-eight patients (20%) died due to transplant complications other than relapse and 47 (24%) experienced a leukemia recurrence. Overall survival (OS) and leukemia-free survivals at 8-years were 55±4% and 53±4%, respectively. Multivariate analysis of factors influencing OS included as covariates age at diagnosis of AML, ELN categories, courses to CR1 and conditioning regimen (MA versus RIC), since they had a p-value <0.1 in the univariate comparisons. The variables with independent on OS impact were age (p=0.01), courses to CR (p=001) and ELN classification (p=0.01). OS at 8 years in the favorable, intermediate I, intermediate II and adverse categories were 69±10%, 53±8%, 69±7% and 42±6%, respectively. In patients from the adverse ELN category, independent factors influencing OS in the multivariate analysis of this subgroup were age (16-60 y-o vs>60, p=0.01) and courses to CR (1 vs more, p=0.03).
The ELN genetic categories have impact on OS of AML patients who receive an ALLOHCT in CR1. The results were very good in the favorable category and, most important, in intermediate II patients. Even patients in the adverse category had a substantial probability of long-term survival. This is remarkable, since the outcome of patients with adverse genetic features when treated with CT only is very poor.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal