Abstract

With recent advances in GVHD prophylaxis, NMA haploBMT has become a viable option for pts who lack a fully matched donor. However, relatively few data are available on disease-specific outcomes following NMA haploBMT. This study evaluated the outcomes of NMA related haploBMT with PT/Cy in pts with lymphoma.
We retrospectively analyzed 151 consecutive pts with poor-risk or advanced lymphoma who received NMA related haploBMT with PT/Cy at Johns Hopkins, without protocol-specified posttransplantation rituximab. Pts had a first-degree related haplo donor (allele or allele-group level typing at HLA-A, -B, -Cw, -DRB1, -DQB1), ECOG PS ≤ 1 or 2, LVEF ≥ 35%, adequate pulmonary and renal function, and in general ≥ PR for aggressive NHL, ≥ SD for Hodgkin lymphoma (HL). Conditioning consisted of Cy (14.5 mg/kg IV, days -6 and -5), fludarabine (30 mg/m2 IV, days -6 to -2), and TBI (200 cGy, day -1) in 98% of cases. Grafts were T-cell replete (bone marrow in 99%). GVHD prophylaxis consisted of high-dose PT/Cy (50 mg/kg IV) either once (day 3; 1 pt) or twice (days 3 and 4; 150 pts), mycophenolate mofetil, and tacrolimus.
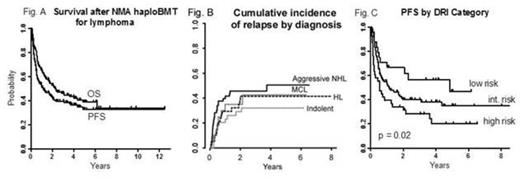
Of the 151 pts (median age 55, range 14-73 y), 52 (34%) had prior autologous BMT. By Disease Risk Index (DRI) categorization (Blood 2012;120(4):905), 38 pts (25%) were high-risk, 89 (59%) intermediate-risk, and 24 (16%) low-risk. There were 38 cases (25%) of HL; 53 cases (35%) of aggressive NHL including 28 B-cell, 24 T-cell, and 1 anaplastic nos; 20 cases (13%) of mantle cell lymphoma (MCL); 39 indolent histologies (17 CLL, 19 FL, 3 other); and 1 case of HL evolved from CLL. With a median follow-up of 3.8 (range 0.5 - 8) y in event-free pts, the 3-y probabilities of both progression-free survival (PFS) and disease-free survival were 40 (95% CI, 32-48)%, with a 3-y overall survival (OS) probability of 46 (39-55)% (figure A). The probability of neutrophil recovery was 88% at day 30 (median 17 days), and the probability of platelet recovery ≥ 20,000/µL was 86% at day 60 (median 26 days). Nonengraftment attributed to primary graft failure or to residual bone marrow malignancy occurred in 17/147 evaluable pts (12%), 8 with CLL. By competing-risk analysis, 1-y probabilities of nonrelapse mortality (NRM) and relapse were 16 (95% CI, 10-22)% and 31 (23-38)%, respectively. The probability of grade 2-4 acute GVHD was 32 (95% CI, 24-39)%, grade 3-4 acute GVHD was 5 (1-8)%, and chronic GVHD was 13 (7-18)%. Disease-specific cumulative incidences of relapse, estimated by competing-risk analysis, are shown in figure B. The 3-y probabilities of PFS and OS were 53 (95% CI, 39-72) and 67 (53-84)%, respectively, in HL; 35 (25-51)% and 38 (26-54)% in aggressive NHL; 23 (9-54) and 28 (13-62)% in MCL; and 42 (29-61)% and 48 (34-67)% in indolent NHL and CLL combined. On unadjusted landmark analyses, we found no statistically significant association between PFS and the development of grade 2-4 acute GVHD treated as a time-independent variable. On unadjusted analysis, the DRI category (low, intermediate, or high) was among the variables statistically significantly associated with PFS (p = 0.02; figure C), and remained independently associated with PFS on multivariate analysis adjusted for pt age (p = 0.002).
NMA related haploBMT with PT/Cy carries acceptable toxicities that parallel those of NMA matched transplants, while producing durable disease control in a clear subset of lymphoma pts. This approach facilitates the integration of new posttransplantation strategies that could reduce the risk of relapse.
Off Label Use: posttransplant cyclophosphamide for GVHD prevention.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal