Abstract

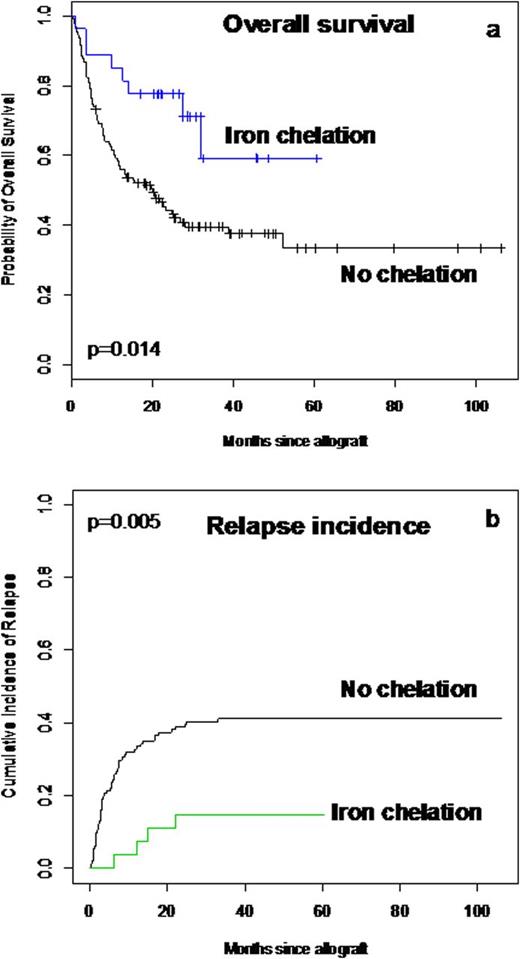
Iron overload (IO), primarily related to multiple red blood cell transfusions, is a relatively common complication in allogeneic hematopoietic stem cell transplant (allo-HSCT) recipients. Elevated pre-transplant ferritin level, a surrogate marker of iron overload, was demonstrated to be an important cause of mortality and morbidity in patients who have undergone allo-HSCT. Excessive iron accumulation results in tissue damage and organ failure, mainly as a result of the generation of free radicals that cause oxidative damage and organ dysfunction. Iron chelators have been widely used leading to normalisation for ferritine level and lower IO-related complications. As iron has a fundamental role in cell survival affecting pathways involved in DNA synthesis, cell differentiation, and apoptosis, some studies evaluated the anti-proliferative activity of iron chelators in cancer and leukemia patients on disease recurrence. The objective of this study was to determine at a first time the impact of serum ferritin level measured at time of allogeneic HSCT in adult patients with hematological disorders on the different outcomes and to investigate at a second time the role of iron chelation on relapse incidence. We included 158 patients, 100 males and 58 females with a median age of 45 years (18-67) who underwent allo-HSCT between 2002 and 2010. There were 83 acute myeloid leukemias, 10 chronic myeloid leukemias, 11 myelodysplastic syndromes, 7 myeloproliferative disorders, 19 myelomas, 9 non-Hodgkin lymphomas, 6 Hodgkin diseases, 5 aplastic anemias and 3 hemoglobinopathies. Sixty-seven (42%) patients were sex mismatched (F→M:37; M→F:30); for ABO compatibility, 61% were compatible, 18% had minor incompatibility and 21% had major incompatibility. Concerning the HSCT procedures, 60 patients (38%) received peripheral blood stem cell and 98 (62%) received bone marrow from 97 (61%) HLA related donors [matched, n=76; mismatched, n=21], and 61 (39%) HLA unrelated donors [matched, n=36; mismatched, n=25] after myeloablative [n=64, (41%)] or reduced intensity conditioning [n=94, (59%)]. At transplantation, 91 (58%) were in complete remission (CR) or chronic phase [CR1: n=61 (67%); ≥CR2: n=30 (33%)]. The median serum ferritin level at HSCT was 1327 microg./l (26-14136); 31(20%) patients had a level 26-500, 33 (21%) had a level 500-2500, and 94 (59%) >2500. There was no significant correlation between the different ferritin levels, disease kind and status at HSCT. After transplantation, 23 patients received iron chelating agents after a serum ferritin level of 1000 microg/l and stopped when the level decreased below 1000. The cumulative incidence of acute GVHD ≥ II at 3 months was 14% (11-16.5) with 10.5% (8-13) for grade III and 7% (5-9) for grade IV; the 1 year cumulative incidence of limited and extensive chronic GVHD were 4% (2-6) and 12.4% (9-16) respectively. After a median follow-up of 18 months (1-106), the 5 years OS probability was 65% for patients with ferritin level below 500 microg./l, 39% for level between 500 and 2500 microg./l and 28% for level > 2500 micog./l, [Hazard ratio= 3.5 (1.5-8.1), p=0.002]; this was explained by a significant higher TRM in patients with level >2500 [Hazard ratio= 4.3 (1.02-18), p=0.04]. Interestingly, we found in multivariate analysis that patients receiving iron chelators had significantly better OS [5 years OS= 59% vs. 34% for non-chelated patients, Hazard ratio= 0.34 (0.15-0.76), p=0.008], (Figure 1a), and experienced less disease relapse [5 years relapse incidence= 18% vs. 41% for non-chelated patients, Hazard ratio= 0.22 (0.07-0.73), p=0.012], (Figure 1b). In conclusion, we confirmed the negative impact of iron overload on the outcomes allo-HSCT recipients. More importantly, we demonstrated that iron chelators have a positive impact in reducing disease relapse by the possible mechanism of iron deprivation in leukemic cells. This clinical observation needs to be confirmed by prospective randomized trials.Close modal
Figure 1
a: Overall survival probability and b: relapse incidence in patients with or without iron chelation
Figure 1
a: Overall survival probability and b: relapse incidence in patients with or without iron chelation
Disclosures:
Michallet:Novartis: Honoraria, Research Funding. Nicolini:Novartis: Consultancy, Honoraria, Research Funding.
Author notes
*
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract
© 2013 by The American Society of Hematology
2013

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal