Abstract
Primary Mediastinal Large B-cell Lymphoma (PMLBCL) is a rare entity corresponding to approximately 10% of all diffuse large B-cell lymphomas (DLBCL), but molecular and clinically distinct. In the pre rituximab (R) era, cyclophosphamide, doxorubicin, vincristine and prednisone (CHOP) chemotherapy, produced inferior results compared to more intense chemotherapy regimens, but improved outcomes were seen with the addition of consolidative radiotherapy (RT). Since the availability of R, there has been a substantial improvement in outcomes, but optimal upfront management, including the role of RT remains undefined. It is unknown if the favorable outcome seen in case series and clinical trials are achievable at the population level. Therefore, we performed a retrospective analysis of a large cohort of non-selected PMBCL patients diagnosed in the pos R era to assess the long-term outcomes and the possible impact of use of RT.
We utilized the National Cancer Institute's Surveillance Epidemiology and End Results (SEER-18) program to identify cases of PMLBCL (International Classification of Diseases-Oncology, Third Edition, ICD-O-3 code 9679/3) diagnosed as first malignant neoplasm. The SEER-18 register includes Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, Utah, Los Angeles, San Jose-Monterey, Rural Georgia, Alaska Native Tumor Registry, Greater California, Kentucky, Louisiana, New Jersey and Greater Georgia. We included all cases reported from 2001 to 2010 and follow up was current up to the end of 2012. Characteristics surveyed included age, sex, stage, race, use of RT, duration of follow up and vital status.
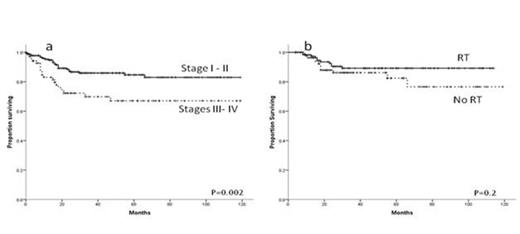
We identified a total of 315 cases of PMBCL. Nine cases were subsequently excluded due to absence of stage information, resulting in 306 patients for analysis with median follow up was 29.5 months (IQR 14.2-60.7). Median age at diagnosis was 36 years (IQR 27-44.7), 183 patients (59.8%) were female, 241 (78.8%) were white and 235 patients (76.8%) had stage I or stage II disease. Overall 3-year survival was 86.4 % (95% C.I. 80.7%-92.1%) for stages I/ II and 71.7% (95% C.I. 57.9% - 85.6%) for stages III/ IV, P=0.002 (Figure, panel a).Of the 298 patients with RT information available, 159 patients (53.3%) received RT as part of their treatment. Among patients with stage I/II disease 122 of the 210 (58%) with information available received RT. There was a trend for higher utilization of RT among male patients with stage I/II disease (65% vs. 54%, P=0.1). There was no significant difference between RT and non-RT patients in terms of age, year of diagnosis and race. Overall 3-year survival was 90.6% (95% C.I. 84.3%-96.9%) for stages I/II patients treated with RT and 83.4 % (95% C.I. 73.1%-93.7%) for the patients who did not receive radiation (Figure, panel b, P=0.2). When adjusted for age, year of diagnosis, race and sex, there was no association between RT and mortality in patients with stage I/II disease.
The high cure rates of PMBCL reported in the R era are reproducible at the population level. We found no evidence that with contemporary systemic treatment the addition of RT produces a positive impact on survival. Prospective trials are necessary to assess the best systemic therapy for PMBCL in the R era and to reevaluate the role of RT in this disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal