Abstract
Hematopoietic stem cells (HSCs) are administered (i) to restore hematopoiesis and immunity in the course of hematopoietic stem-cell transplantation (HSCT), (ii) as a replacement for inherited blood disorders and bone marrow failure, (iii) to regenerate cells of alternative lineages for restorative medicine, and (iv) as a source for generating specific hematopoietic cells (e.g., T cells, NK cells, and dendritic cells). However, the widespread application of allogeneic HSCs for humans is hampered by their immune-mediated destruction by host T cells recognizing mismatched HLA or by HLA-specific antibodies. Despite pre-banking umbilical cord blood (UCB) units and access to adult donors through the National Marrow Donor Program (NMDP), finding a suitable HLA-matched product is challenging for many recipients, especially those from ethnic minorities who are under-represented in the donor pool. The available donor pool would be markedly increased if donor HSCs were edited to eliminate expression of the HLA-A locus. Indeed, modeling from NMDP shows that the chance of an African American recipient finding a HLA-matched donor increases from 18% to 73% when matched for HLA-B, C and DR, instead of HLA-A, B, C and DR. We have previously shown that engineered zinc finger nucleases (ZFNs) can disrupt HLA-A expression in genetically edited T cells (Blood 2013). To extend this proof-of-concept to HSCs, we sought to disrupt HLA-A expression by introducing ZFNs targeting this locus. CD34+lineageneg HSCs (99% purity) were isolated using paramagnetic beads from UCB. Electro-transfer of in vitro transcribed mRNA encoding the HLA-A-specific ZFN generated 30% HLA-Aneg HSCs after one week ex vivo culture with defined cytokines (FLT3-L, SCF, TPO, and IL-6) and an aryl hydrocarbon receptor antagonist (stem reginin-1, SR-1). As expected, SR1 treatment maintained greater numbers of CD34+ cells (also CD34posCD38neg) in culture compared to controls. DNA sequence analysis revealed that HLA-Aneg HSCs encode the expected nucleotide changes at the ZFN target site. An in vivo engraftment assay, using NOD.Cg-PrkdcscidIl2rgtm1Wjl/SzJ (NSG) mice, demonstrated that HLA-Aneg HSCs maintain the capability of engraftment and differentiation into HLA-Aneg hematopoietic cells (Figure ). Thus, disruption of HLA-A expression in HSCs provides an appealing approach to increasing the chances for of finding HLA-matched donors and may broaden the clinical application of allogeneic HSCT. Furthermore, the ability to genetically edit HSCs has implications for (i) preventing immune-mediated recognition of HLA-disparate HSC and (ii) preventing immune mediated recognition of self-antigens.
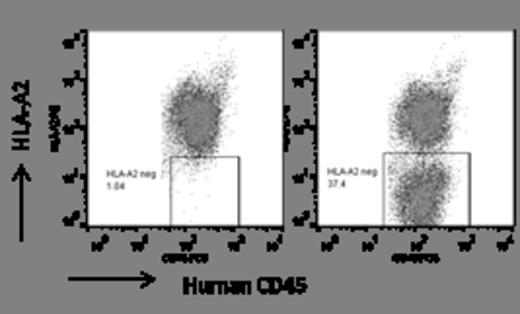
Engraftment of HLA-A2neg HSCs was evaluated in vivo. Data shown are flow-cytometry analysis of bone marrow obtained from NSG mice 16 weeks after HSC injection. HSC engraftment and HLA-A2 expression in NSG mice injected with un-modified HSCs (left panel) and HSCs treated with the HLA-A specific ZFNs (right panel) are shown. Data are gated on human CD45 positive cells.
Reik:Sangamo BioSciences: Employment. Holmes:Sangamo BioSciences: Employment. Gregory:Sangamo BioSciences: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal