Abstract

MAGE-A3 is a cancer-testis antigen expressed in various human cancers, including MM, but not in normal non-gonadal tissues. MAGE-A3 expression inhibits apoptosis in MM cells, and has been associated with a more aggressive clinical course, making it a rational target for immunotherapy. Pre-autoSCT myeloablative conditioning provides tumor antigen release and a lymphopenic environment that may be ideal for expansion of primed PBL and generation of anti-myeloma immune responses.
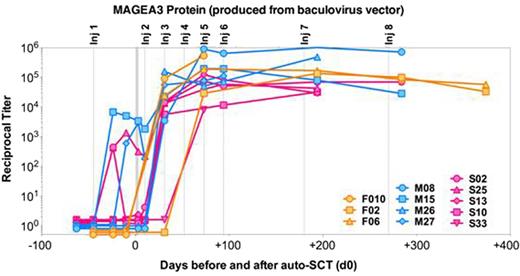
Eligibility for this pilot study required symptomatic MM within 1 year of diagnosis; MAGE-A+ MM cells by immunohistochemistry (IHC); at least VGPR following induction therapy; and meeting institutional criteria for autoSCT. The immunotherapy consists of a recombinant protein containing full-length MAGE-A3 fused to part of H. influenzae Protein D antigen, mixed with the AS15 immunostimulant (containing MPL, QS21, and CpG7909). Six weeks prior to SCT, patients received their 1st injection (300 µg recMAGE-A3 intramuscularly), followed 3 weeks later by steady-state leukopheresis to collect primed PBL. They then underwent stem cell mobilization and a melphalan 200 mg/m2-conditioned autoSCT, followed by re-infusion of unmanipulated PBL on day +3 after SCT, and 7 post-SCT injections (days +10, 31, 52, 73, 94, 180, and 270). Lenalidomide maintenance was permitted. The primary objectives were safety and tolerability. The secondary objectives were cellular and humoral immune responses and clinical outcomes. Humoral immunity was assessed by ELISA using baculovirus-generated recombinant MAGE-A3 protein.
Of 93 pre-screened patients, 30 (32%) were MAGE-A+ by IHC. Of these, 13 (43%) enrolled. Reasons for non-enrollment were: did not achieve VGPR (n=6), declined/received other therapy (n=7), other (n=4). For enrolled patients, median age was 56; ISS stages I/II/III were 58%/25%/17%; 45% had high-risk cytogenetics at diagnosis (n=11 tested). Responses at enrollment were 12 VGPR and 1 CR; most (83%) had received VRD-based induction. All patients had adequate PBL collections (median 1.4 x 108 CD3+ cells/kg, range 1.0-2.6), and all collected stem cells successfully (median 11.4 x 106 CD34+ cells/kg, range 8.3 – 37.2). Autologous PBL infusions were well-tolerated, with no engraftment-like syndromes. Time to neutrophil recovery (median 11 days) and SCT-related toxicities were typical. The immunotherapy schedule was feasible with only 1 missed dose to date. Potential immunotherapy-related AE's (all grade 1 or 2) include injection site pain/reaction (n=6), myalgia/flu-like symptoms (n=5), fever/chills (n=2), fatigue (n=1), and rash (n=1). Three SAE's were observed: 1 immunotherapy-related (grade 2 myalgia requiring a 24-hour hospitalization), and 2 unrelated (grade 3 diarrhea, grade 3 atrial fibrillation with pulmonary edema). There have been no autoimmune toxicities and no deaths on study. Four patients initiated lenalidomide maintenance with no unexpected toxicities. Regarding immune responses, 12 of 12 (100%) evaluable patients have developed high-titer (>104) IgG antibodies against MAGE-A3 (Fig.). Responses were seen in all but 2 patients by day +31 post-SCT, and in all patients by day +75, persisting at 1 year post-SCT in both patients reaching this timepoint so far. All patients also developed strong IgG responses against Protein D. Clinically, at 3 months post-SCT, 50% of patients had achieved CR (33% stringent CR). With a median follow-up of 10 months post-SCT (range 1-20), 92% are progression-free, with follow-up ongoing.
MAGE-A3 protein immunotherapy plus autologous PBL transfer is feasible, has an acceptable safety profile, and is strongly immunogenic, capable of overcoming the profound immune suppression typically seen in MM patients post-autoSCT. The presence of IgG-type anti-MAGE antibodies implies the generation of a CD4 T cell response to induce Ig class-switching, though formal assessment of T cell responses against MAGE-A3 and other antigens are needed to confirm this, and are ongoing. Importantly, the use of an “off-the-shelf” immunotherapy product and unmanipulated autologous PBL transfer allows the treatment to be given at any transplant center. Further study of this approach as a strategy to consolidate post-autoSCT responses and potentially eliminate minimal residual disease is warranted.
Bristol Meyers Squibb: Honoraria, Research Funding; Celgene: Membership on an entity’s Board of Directors or advisory committees; Onyx: Honoraria; Millennium: Honoraria. Bertolini:Ludwig Institute for Cancer Research: Employment. Pan:Ludwig Institute for Cancer Research: Employment. Venhaus:Ludwig Institute for Cancer Research: Employment. Fellague-Chebra:GlaxoSmithKline Vaccines: Employment. Gruselle:GlaxoSmithKline Vaccines: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal