Abstract
Tyrosine kinase inhibitor (TKI) induced neutropenia and thrombocytopenia may be relieved with G-CSF and trombopoietin analogs. To characterize the signaling response in a CML patient treated with hematopoietic growth factors and TKI, we employed single cell analysis of phosphoproteins in serial samples.
We characterized the single cell phosphoprotein responses to treatment with dasatinib, eltrombopag, and pegfilgrastim in CML-like cell lines K562 and KCL-22, normal peripheral blood leukocytes and leukocytes from a patient starting on nilotinib. These data formed a basis for comparison with serial samples (Figure 1) from a CML patients after extensive wash-out before restarted on third-choice TKI, combined with eltrombopag and pegfilgrastim. For characterization of in vivo transformational potential CML patient bone marrow cells were engrafted in duplicate in NOG mice by femoral injection. Basal phosphorylation was determined using 17 phosphorylation specific antibodies: All staining panels contain the same 4 surface antibodies and a live-dead discriminator; CD33(P67.6) PerCP-Cy5.5, CD38(HB7) PE-Cy7, CD34(581) PE, CD45(MEM-28) PE-Dynamics590 and phospho c-PARP(Asp214) AlexaFlour-700. Two phosphospecific antibodies were added to each panel with the respective direct conjugated dye Alexa Flour 488 and Alexa Flour 647. The lowest median signal for each phosphoprotein in CML cells and lymphocytes, respectively, were used as reference value for calculation of basal phosphorylation.
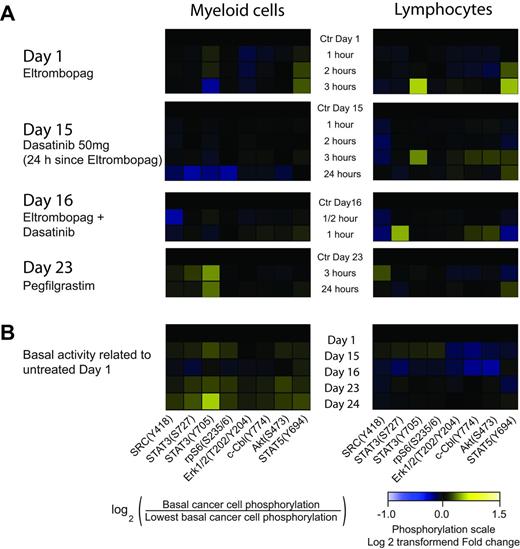
Single cell phosphorylation status of myeloid and lymphatic cells collected from CML patient, treated with dasatinib, eltrombopag, and pegfilgrastim.
Single cell phosphorylation status of myeloid and lymphatic cells collected from CML patient, treated with dasatinib, eltrombopag, and pegfilgrastim.
A 56 y old male was diagnosed with CML (Sokal RR 0.75, Hasford RR 929, karyotype 46,XY,t(9;22)(q34;q11)[20], FISH 9q34 ABL/22q11.2 BCR dual fusion 62% of cells, PCR positive BCR-ABL e13e2/e14a2), developed prolonged thrombocytopenia and neutropenia on various dose levels of imatinib and nilotinib (neutrophile <1x109/L, <30x109/L) during the first 7 months after diagnosis. After a 6 months pause of TKI therapy: quantitative PCR BCR-ABL1/ABL1 25%IS, bone marrow biopsy with reduced normal megakaryocytes. Platelet supportive therapy with eltrombopag 50 mg daily was initiated 14 days before start with dasatinib 50 mg daily keeping platelet level above 50. After two more weeks pegfilgastim 6 mg was started, increasing neutrophils above 1.0x109/L.
The CML bone marrow engrafted without symptomatic disease in NOG mice over 6 months monitoring, in contrast to engraftment with disseminated disease in an accelerated phase CML patient sample and the KCL-22 cell line. Phosphorylation of patient myeloid cells indicated STAT3(pY705) and STAT5(pY694) phosphorylation 2 and 3 hours after intake of eltrombopag. Dasatinib modestly inhibited SRC(pY418) and STAT3(pY705), but only transiently blunted the effect of eltrombopag. Pegfilgrastim strongly induced STAT3(pY705), STAT3(pS727), and SRC(pY418). Further analyses of cellular subsets and phospho-Abl will be presented.
Eltrombopag kept stable levels of platelets on dasatinib treatment, and cell phosphorylation reflected persisting signaling induced by eltrombopag after seven days on combination therapy. Pegfilgrastim induced strong phosphorylation of STAT3(pY705) during dasatinib co-therapy. Phosphoprotein signal analysis of patient leukemic cells reflected the hematological response of dasatinib, eltrombopag, and pegfilgrastim and may be used to monitor therapy responses of and growth factors and targeted therapy.
Phosphoprotein modulated early after start of treatment. (A) Each day 1-23 is analysed separately with its pretreatment sample as control and signal baseline. (B) Various treatment days are compared, using pretreatment control at day 1 used as baseline. (A) and (B) were analysed by flow cytometry at the same day, using bar code labelling, sample processing and analysis as previously described (Skavland et al. Blood Cancer J 2012). On day 16 dasatinib and eltrombopag is administrated concomitantly. Signalling responses in lymphocytes were distinct different from myeloid cells. Further determination of cellular subsets and their signalling responses will be presented.
Popa:KinN Therapeutics AS: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal