Abstract
NK cells are primary effectors of the innate immune response against cells that have undergone malignant transformation. Several lines of evidence indicate that the expression level of NK ligands on leukemic cells affects the sensitivity of the leukemic cells to cytolytic activity by NK cells. Various agents have been evaluated for their ability to induce these ligands on leukemic cells to augment the NK cell mediated anti-leukemia effect.
There is substantial evidence that has established the importance of the adaptive immune system in the treatment of acute promyelocytic leukemia (APL) (Rose Ann Padua et al. Nat Med 2003). While there is significant data which address the mechanisms of arsenic trioxide (ATO) on malignant promyelocytes, limited data is available of its effect on the innate and adaptive immune system. We undertook a series of experiments to address the impact of ATO on NK cell receptor and malignant promyelocyte ligand expression and its effect on NK cell mediated cytotoxicity. We also evaluated NK cell reconstitution in patients treated with ATO and the impact of KIR genotypes on relapse.
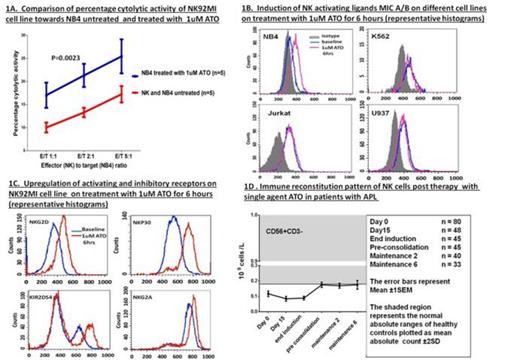
We first evaluated the cytotoxic activity of NK92MI (NK cell line) against 5 different myeloid (K562, U937, HL60, UF1, NB4) and 2 lymphoid cell lines (Jurkat E6.1, SUP-B15) by CFSE/ 7AAD cytotoxicity assay. Target (T) cells (1x 105/100 µL/well) pre-treated with CFSE were co-cultured with effector NK cells (E) at a E:T ratio of 1:1, 2:1 and 5:1 for 5 hours at 37°C in 96 well plates. The percentage cytolytic activity of the NK cells was then calculated after adding 7AAD and acquired in FACS Calibur (Becton Dickinson, San Jose, CA, USA). Significant cytolytic activity was noted against K562 and NB4 cell lines. At the highest E:T ratio there was a median 22% cytolytic activity against NB4 (N=5). We observed that NB4 when treated overnight with 1µM ATO (>99% viability retained after this exposure) significantly increased the cytotoxic effect of NK92MI cell line at all the E:T ratios as shown in figure 1A (n=5; P=0.0023). No other cell line showed a similar increase in cytotoxic effect following exposure to ATO at these concentrations (data not shown).
We next evaluated the effect of exposure of NB4 cells to ATO at 1µM for 6 hours on NK ligand expression by flowcytometry. As shown in figure 1B there was a significant increase in activating ligand MICA/B in NB4 cell lines (n=3; P=0.016) which was not seen in any of the other cell lines. Similar significant increased expression of Nectin-2 (DNAM-1 ligand) and HLA Class I was seen. Exposure of NK92MI to ATO for 6 hours at 1uM (non cytotoxic dose:IC50-3.8uM) resulted in increased expression of activating receptors NKG2D, NKP30 and KIR2DS4 (figure 1C) and inhibitory receptor NKG2A and decrease in inhibitory receptors KIR3DL1/DL2. There were no changes in the expression of NKP46, KIR2DL1, KIR2DL2 and DNAM1 receptors.
We undertook a prospective study to evaluate the pattern of NK (CD56+CD3-) reconstitution in patients with newly diagnosed APL treated at our center with a single agent ATO regimen (Mathews et al. JCO 2011). The mean NK cell counts in patients were below the 2SD deviation level of the normal range even after completion of therapy (approximately a year)(figure 1D). All other subsets evaluated (CD4, CD8, CD3, CD19, CD56+CD3+, CD4CD45RO) had returned to levels within the normal range by the end of consolidation therapy (approximately 3 months from diagnosis).
KIR genotyping was done on 55 patients with APL who received treatment with single agent ATO based regimen. The median follow up of this cohort was 20 months and 14 cases relapsed following initial therapy. The presence or absence of 17 KIR genes was done by PCR-SSP method (KIR Typing kit, Miltenyi Biotech Inc, CA). There was no association with any specific genotype or haplotype with risk of relapse.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal