Abstract
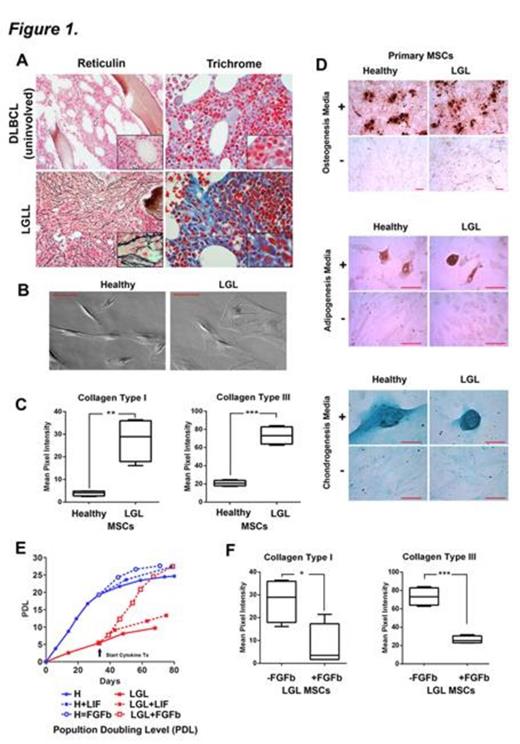
Large Granular Lymphocyte (LGL) leukemia is associated with chronic lymphoproliferation in association with unexplained cytopenias. Discovery of somatic mutations in STAT3 provides new insights into the molecular basis of LGL leukemia, but the precise mechanism leading to cytopenias remains unresolved. To gain insight into this mechanism, bone marrow fibrosis (Fig. 1A) was found to occur in 88% of cases and is significantly associated with splenomegaly, the presence of cytopenias, and co- existence of autoimmune diseases. In this study, we are reporting the identification of the fibrosis initiating cell population.
Primary mesenchymal stromal cultures (MSCs) from LGL leukemia BM were isolated and grown under reduced oxygen conditions using undifferentiated and differentiation-specific culture conditions (Fig. 1B). These cultured cells were confirmed to deposit greater amounts of fibrillar Type I, III and V collagen matrix consistent with the heavy reticulin and trichrome positive stains observed in bone marrow biopsies (Fig. 1C). This collagen-producing cell population failed to support normal hematopoietic progenitor proliferation and colony formation in co-culture assays. Microarray analysis of the collagen-producing mesenchymal cell population was conducted and pathway analysis was performed using the GeneGo analysis platform from MetaCore™. Each list of genes was individually grouped and evaluated for membership on the set of GeneGo® pathway maps under the functional ontology enrichment tool. Calculation of p-values using hypergeometric distribution was used to determine pathway statistical significance. Flow cytometry was conducted to further evaluate the mesenchymal lineage.
Supervised hierarchical clustering was performed to determine the overall similarity of LGL MSCs to publicly available, platform-compatible, microarrays from cells of mesenchymal lineage. Clustering showed that both patient and control MSCs display expression patterns distinct from committed mesenchymal lineages including osteoblasts, chondrocytes, and adipocytes. Mesenchymal-derived fibroblast differentiation can be distinguished by down-regulated CD29, CD44, CD105, CD106, CD117, bone morphogenetic protein receptor, and Sca-1 expression, and by up-regulated collagen type I, collagen type III, tenacin C, fibronectin, matrix metalloproteinase 1, fibroblast-specific protein 1, and vimentin. By microarray analysis and flow cytometry, we find no evidence that the cells are differentiated cells aside from collagen over expression. In order to define their pluripotent potential, sub-confluent cultures were grown in three types of differentiating media. Primary MSCs from both LGL leukemia patients and healthy controls were similar in their capacity to undergo trilineage differentiation into osteoblasts (stained with Alizarin Red S), adipocytes (Oil red O), and chondrocytes (Alican blue) (Fig. 1D). Next, pathway analyses revealed significant re-programming of the pluripotent MSCs. ECM production pathways were increased while proliferation pathways were down-regulated. Proliferation of MSCs is governed by production of autocrine growth factors. Both leukemia inhibitor factor (LIF) and basic fibroblast growth factor (FGFb) were significantly reduced compared to control MSCs (p<0.001) and the proliferative capacity of the LGL MSCs was severely diminished. Exogenous FGFb, but not LIF, restored LGLL MSC proliferation comparable to normal MSCs (Fig. 1E), normalized their spindle-shaped morphology, and maintained MSC plasticity. Interestingly, treatment with exogenous FGFb normalized collagen deposition (Fig. 1F) and restored hematopoietic supporting function.
STAT-activated LGL leukemia cells, like myeloproliferative neoplasms, share a propensity for the development of bone marrow fibrosis. These results indicate that MSCs from LGL leukemia are pluripotent, but are re-programmed to deposit excessive amounts of collagen. Restoration of FGFb maintains the pluripotency of these MSCs while reversing the fibrosis phenotype. Our data suggests that FGFb-cultured MSCs may be used to reverse cytopenias in LGL leukemia.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal