A 79-year-old woman presented with new-onset weight loss, bilateral axillary lymphadenopathy (LAD), and a chest wall mass. A complete blood count showed a leukocytosis of 87 600/μL with 99% lymphocytes. A review of the peripheral blood smear and flow cytometry (data not shown) showed chronic lymphocytic leukemia (CLL).
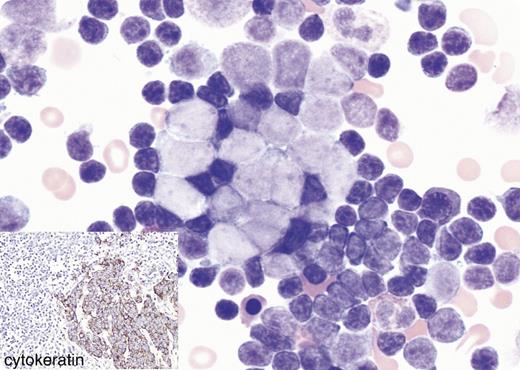
Due to B symptoms, LAD, and a chest wall mass, a Richter transformation (RT) of the CLL was highly suspected. The bone marrow aspirate revealed extensive marrow involvement by CLL. In addition, there were many large cells with oval nuclear contours and open chromatin. These cells were arranged singly or in small cohesive clusters.
While RT was within the differential diagnosis, a metastatic carcinoma was preferred. The bone marrow biopsy specimen (data not shown) showed that in the background of CLL was the focal infiltrate of a sheet of cohesive pan-cytokeratin–positive large cells (see insert) that were negative for B-cell antigens, including PAX-5. The excisional chest wall and axillary lymph node biopsy specimens showed a Merkel cell carcinoma (MCC) and a metastatic MCC, respectively.
Approximately 94% of MCCs are positive for PAX-5, which can lead to an erroneous diagnosis of RT if only PAX-5 immunohistochemistry is chosen. However, the MCC in this case was negative for PAX-5.
A 79-year-old woman presented with new-onset weight loss, bilateral axillary lymphadenopathy (LAD), and a chest wall mass. A complete blood count showed a leukocytosis of 87 600/μL with 99% lymphocytes. A review of the peripheral blood smear and flow cytometry (data not shown) showed chronic lymphocytic leukemia (CLL).
Due to B symptoms, LAD, and a chest wall mass, a Richter transformation (RT) of the CLL was highly suspected. The bone marrow aspirate revealed extensive marrow involvement by CLL. In addition, there were many large cells with oval nuclear contours and open chromatin. These cells were arranged singly or in small cohesive clusters.
While RT was within the differential diagnosis, a metastatic carcinoma was preferred. The bone marrow biopsy specimen (data not shown) showed that in the background of CLL was the focal infiltrate of a sheet of cohesive pan-cytokeratin–positive large cells (see insert) that were negative for B-cell antigens, including PAX-5. The excisional chest wall and axillary lymph node biopsy specimens showed a Merkel cell carcinoma (MCC) and a metastatic MCC, respectively.
Approximately 94% of MCCs are positive for PAX-5, which can lead to an erroneous diagnosis of RT if only PAX-5 immunohistochemistry is chosen. However, the MCC in this case was negative for PAX-5.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal