Key Points
After recovering from TTP, the prevalence of hypertension, depression, and systemic lupus erythematosus and risk of death are increased.
TTP may be a more chronic disorder rather than a disorder of acute episodes and complete recovery.
Abstract
Recovery from acute episodes of thrombotic thrombocytopenic purpura (TTP) appears complete except for minor cognitive abnormalities and risk for relapse. The Oklahoma TTP-HUS (hemolytic uremic syndrome) Registry enrolled 70 consecutive patients from 1995 to 2011 with ADAMTS13 activity <10% at their initial episode; 57 survived, with follow-up through 2012. The prevalence of body mass index (BMI), glomerular filtration rate (GFR), urine albumin/creatinine ratio (ACR), hypertension, major depression, systemic lupus erythematosus (SLE), and risk of death were compared with expected values based on the US reference population. At initial diagnosis, 57 survivors had a median age of 39 years; 45 (79%) were women; 21 (37%) were black; BMI and prevalence of SLE (7%) were greater (P < .001) than expected; prevalence of hypertension (19%; P = .463) was not different. GFR (P = .397) and ACR (P = .793) were not different from expected values. In 2011-2012, prevalence of hypertension (40% vs 23%; P = .013) and major depression (19% vs 6%; P = .005) was greater than expected values. Eleven patients (19%) have died, a proportion greater than expected compared with US and Oklahoma reference populations (P < .05). TTP survivors may have greater risk for poor health and premature death.
Continuing Medical Education online
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education through the joint sponsorship of Medscape, LLC and the American Society of Hematology.
Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 70% minimum passing score and complete the evaluation at http://www.medscape.org/journal/blood; and (4) view/print certificate. For CME questions, see page 2142.
Disclosures
Johanna A. Kremer Hovinga, Bernhard Lämmle, and James N. George are consultants for Baxter, Inc. for the development of rADAMTS13 as a potential treatment of thrombotic thrombocytopenic purpura (TTP). James N. George is a consultant for Alexion, Inc. for eculizumab as treatment of aHUS. The Associate Editor Leslie V. Parise has served as an advisor or consultant for Bayer, BD Technologies, Biogen, and the Blood Research Institute of Wisconsin; has received grants for clinical research from the Doris Duke Charitable Foundation and the American Heart Association; and owns stock, stock options, or bonds from Covidien, Pfizer, Proctor and Gamble, and Intuitive Surgical. The remaining authors and CME questions author Laurie Barclay, freelance writer and reviewer, Medscape LLC, declare no competing financial interests.
Learning objectives
Identify clinical characteristics of patients with thrombotic thrombocytopenic purpura (TTP) at their initial diagnosis.
Describe the long-term morbidity and mortality of patients with TTP.
Release date: September 19, 2013; Expiration date: September 19, 2014
Introduction
Thrombotic thrombocytopenic purpura (TTP) is an uncommon disorder characterized by acute episodes of systemic microvascular thrombosis.1 Mortality from TTP was 90% in the era before effective treatment2 ; with the use of plasma exchange (PEX) treatment in the 1980s, mortality decreased to 20%.3 Recovery from acute episodes appeared to be complete except for a risk for recurrent acute episodes.4,5
Continuous comprehensive long-term observations of all patients following recovery from their initial acute episode of TTP or hemolytic uremic syndrome (HUS) is a principal goal of the Oklahoma TTP-HUS Registry, an inception cohort of consecutive patients established in 1989.5,6 Support group meetings began in 1996 as part of patient follow-up.7,8 Discussions at these meetings revealed that many patients felt their recovery had been incomplete; they had persistent problems with memory, concentration, and endurance. The clinical importance of these symptoms was supported by documentation of significant deficits in both physical and mental health domains of the Short Form-36 (SF-36), a standard health-related quality-of-life assessment.9 Documentation of minor but significant abnormalities of cognitive function suggested a basis for these problems.10
This report describes our follow-up through 2012. We focused on patients who had recovered from TTP associated with acquired, severe ADAMTS13 deficiency, which identifies a demographically distinct cohort11,12 whose autoimmune etiology and risk for relapse suggested a potentially greater risk for long-term morbidity. Patients were assessed for depression because depression can also affect memory, concentration, and endurance and because TTP survivors’ mental health quality-of-life scores were abnormal.9 Because the abnormal cognitive function10 was postulated to result from residual neurologic ischemic injury, kidney function was measured to determine if there was also evidence for chronic kidney injury. To control for other etiologies of chronic kidney disease, we documented the presence of hypertension and diabetes. These long-term follow-up observations revealed unexpected major morbidities and premature death.
Patients and methods
The Oklahoma TTP-HUS Registry
The Oklahoma TTP-HUS Registry, established January 1, 1989, is a prospective, population-based inception cohort of all consecutive patients identified by a request to the Oklahoma Blood Institute (OBI) for PEX treatment of a diagnosis of TTP or HUS.5,6 The OBI is the sole provider of PEX for all hospitals in 58 of Oklahoma’s 77 counties, and PEX treatment is the standard of care for all patients diagnosed with TTP and is also requested for some patients diagnosed with HUS. Therefore all patients with an initial diagnosis of TTP, without selection or referral bias, are enrolled in the Registry. Serum has been collected immediately before the first PEX beginning November 13, 1995. ADAMTS13 activity was measured by both quantitative immunoblotting and fluorogenic assay using FRETS-VWF73 substrate; severe ADAMTS13 deficiency was defined as activity <10% by either method.5 The Registry is approved by the institutional review boards of the University of Oklahoma Health Sciences Center and all participating hospitals for continuous follow-up of all patients. Patients gave informed consent in accordance with the Declaration of Helsinki.
Follow-up patient evaluations
All patients were observed at least once per year by phone or mail as well as at support group meetings. Beginning in 2004, we saw patients whose initial episode was associated with severe ADAMTS13 deficiency for annual examinations and laboratory evaluation, including ADAMTS13 measurements. Because outcomes were assessed by using data obtained at different times, durations of follow-up are not the same for all outcome assessments. Hypertension, diabetes, and systemic lupus erythematosus (SLE) were documented by the requirement for regularly prescribed medications for these disorders. Glomerular filtration rate (GFR) was estimated by the Chronic Kidney Disease-Epidemiology Collaboration (CKD-EPI) equation13,14 from the most recent serum creatinine measurement. Microalbuminuria was quantified by measurement of the albumin/creatinine ratio (µg albumin/mg creatinine) on a random urine sample taken during the annual evaluation. Depression was assessed by the Patient Health Questionnaire 8 (PHQ-8), which asks about depressive symptoms during the previous 2 weeks.15 Cause of death was determined by autopsy (when performed), from hospital records (when a patient died while hospitalized), or from the death certificate.
Statistical analysis
For the morbidity outcomes, indirect standardization methods16 were used to determine the expected value of each outcome based on the specific rates from the National Health and Nutrition Examination Survey (NHANES) US reference population. Patient data were compared with expected percentages by using one-way χ2 analysis (or exact methods, if the assumptions were not met). For mortality, indirect standardization methods16 were used to determine the expected risk of death based on data from the Centers for Disease Control and Prevention (CDC). Patient mortality was compared with the expected values based on the US and Oklahoma reference populations by using Kaplan-Meier methods with point-wise limits. All analyses were performed by using SAS 9.2 and α = .05.
Reference populations.
To compare patient data to the NHANES reference population, age was categorized by 10-year increments. Race was categorized into black and white (2 Native American patients were categorized as white; there were no other races). Body mass index (BMI) was categorized into <35 kg/m2 and ≥ 35 kg/m2, since this is an important distinction for mortality.17
Hypertension, diabetes, and kidney function.
Expected values were calculated by using data from six 2-year cycles (1999-2010) of NHANES data. We controlled for the potential confounding effects of age, race, gender, and BMI. Comparable to NHANES, we collected the point prevalence of hypertension and diabetes over a 2-year period (2011-2012).
SLE.
Expected values were calculated by using data from NHANES III (1988-1994), which has data for SLE. We controlled for the potential confounding effects of age, race, and gender; there were too few patients in the NHANES data to also control for BMI.
Depression.
Expected values were calculated by using data from the three cycles (2005-2010) of NHANES, with data on depression defined by the PHQ-8. We controlled for the potential confounding effects of age, race, gender, and BMI.
Mortality.
Data for the reference population were obtained from the CDC (1999-2010). CDC estimates the probability of survival for the United States and for each state by 1-year age groups for race and gender by using death certificate and census population data. Life expectancy for individual patients was based on the patient’s age (at the time of initial TTP diagnosis), race, and gender and was determined from the CDC Life Table for the year of their initial TTP diagnosis.
Results
Patients
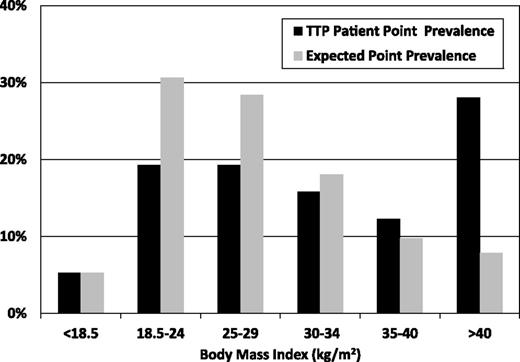
From 1995, when systematic collection of serum samples before beginning PEX treatment began, through 2011, 311 (93%) of 333 patients enrolled for their first episode of clinically diagnosed TTP or HUS had ADAMTS13 activity measurements. ADAMTS13 activity was <10% in 70 patients (23%). Fifty-seven (81%) of these 70 patients survived their initial episode of TTP; they are the subjects of this study. Of these 57 patients, 46 were characterized as idiopathic, 3 were postpartum, 2 presented with bloody diarrhea, 4 had a previous diagnosis of SLE, and 2 had a systemic infection that may have caused their presenting clinical features.5,6 All 57 patients had acquired ADAMTS13 deficiency documented by ADAMTS13 inhibitor activity or recovery of ADAMTS13 activity during remission.5 At the time of their initial episode, median age was 39 years (range, 9 to 71 years), 45 (79%) were women, and 21 (37%) were black. Their BMI was significantly greater than the expected US values (P < .001; Figure 1). Individual data for all 57 patients are presented in supplemental Table S1 (available on the Blood Web site).
BMI of the 57 patients who survived their initial episode of TTP. Data are from the time of their initial diagnosis of TTP. Black bars represent patients; gray bars represent the expected prevalence based on age, race, and gender-specific rates from the NHANES US reference population. Patients’ BMI during follow-up was not different from initial values (n = 52; median follow-up, 5.7 years; range, 0.2 to 16.5 years; P = .922).
BMI of the 57 patients who survived their initial episode of TTP. Data are from the time of their initial diagnosis of TTP. Black bars represent patients; gray bars represent the expected prevalence based on age, race, and gender-specific rates from the NHANES US reference population. Patients’ BMI during follow-up was not different from initial values (n = 52; median follow-up, 5.7 years; range, 0.2 to 16.5 years; P = .922).
Follow-up evaluations
Beginning in 2004, 49 patients (86%) were seen 1 to 7 times (median, 5 times) for annual follow-up evaluations. Not all patients attended the follow-up evaluations every year. We have not seen and have no medical records for 1 patient (#36; supplemental Table S1) since his initial TTP episode; however, we know by regular phone contact with his family that he is alive and has not relapsed. Data for the other 7 patients who have not been evaluated (3 died before 2004; 4 have not participated) were obtained from our follow-up records, hospital records, and records from their primary care physicians. One patient (#52; supplemental Table S1) was lost to follow-up after 4.3 years.
ADAMTS13 activity during remission
The natural history of ADAMTS13 activity during remission was determined from measurements during our annual follow-up evaluations. Among all 49 patients, 24 (49%) had consistently normal activity (≥50%) on 1 to 7 measurements (median, 4 measurements). Twelve patients (24%) had activity of 10% to 49% on 1 or more measurements but had no values <10%; 8 of these 12 patients also had one or more values of ≥50%. Thirteen patients (27%) had activity <10% on 1 to 6 measurements (median, 2 measurements); 9 of the 13 patients also had 1 or more values ≥50%. Patients with ADAMTS13 activity <10% during remission were observed without treatment. Eleven of these 13 patients have not had a subsequent relapse with follow-up of 0.5 to 9 years (median, 3 years); 2 patients have had values <10% for 3 and 7 years at each measurement and have not relapsed; 1 patient had values <10% for 4 years at each measurement and then relapsed 16 months after her last measurement. In the other patient who relapsed following a measurement of ADAMTS13 activity <10% during remission, the relapse occurred 32 months after her last measurement.
Relapse
Twenty-one (37%) of the 57 surviving patients have had 1 to 4 relapses (median, 1 relapse). Nine of these 21 patients had ADAMTS13 activity measured during remission preceding a relapse; the measurement preceded a relapse by less than 3 months in only 2 of these 9 patients. In 1 patient, ADAMTS13 activity was 14% 31 days preceding a relapse; in the other patient, ADAMTS13 activity was 30% 51 days preceding a relapse.
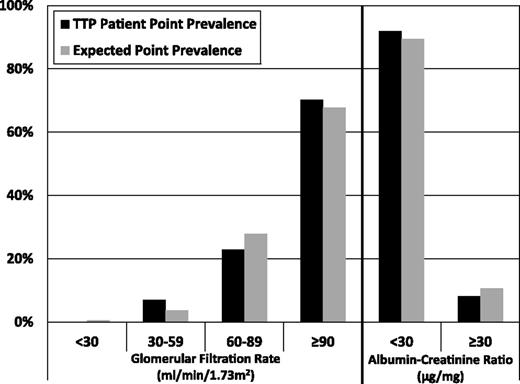
Kidney function
GFR, estimated in all 57 patients at the time of their last follow-up (median, 5.3 years; range, 0.1 to 15.7 years), was not different from the expected values (P = .397; Figure 2). Albumin/creatinine ratio, measured in 37 (80%) of the 46 surviving patients in 2011 (median follow-up, 5.9 years; range, 1.1 to 15.7 years) was also not different from the expected values (P = .793; Figure 2).
Kidney function following recovery from TTP. GFR, estimated by the CKD-EPI equation13,14 in all 57 patients at the time of their most recent serum creatinine measurement (median follow-up, 5.3 years; range, 0.1 to 15.7 years), was not different from the expected prevalence based on age, race, gender, and BMI-specific rates from the NHANES US reference population (P = .397). The albumin/creatinine ratio was measured in 2011 on 37 (80%) of 46 surviving patients (median follow-up, 5.9 years; range, 1.1 to 15.7 years); it was also not different from the expected prevalence based on age, race, gender, and BMI-specific rates from the NHANES US reference population (P = .793).
Kidney function following recovery from TTP. GFR, estimated by the CKD-EPI equation13,14 in all 57 patients at the time of their most recent serum creatinine measurement (median follow-up, 5.3 years; range, 0.1 to 15.7 years), was not different from the expected prevalence based on age, race, gender, and BMI-specific rates from the NHANES US reference population (P = .397). The albumin/creatinine ratio was measured in 2011 on 37 (80%) of 46 surviving patients (median follow-up, 5.9 years; range, 1.1 to 15.7 years); it was also not different from the expected prevalence based on age, race, gender, and BMI-specific rates from the NHANES US reference population (P = .793).
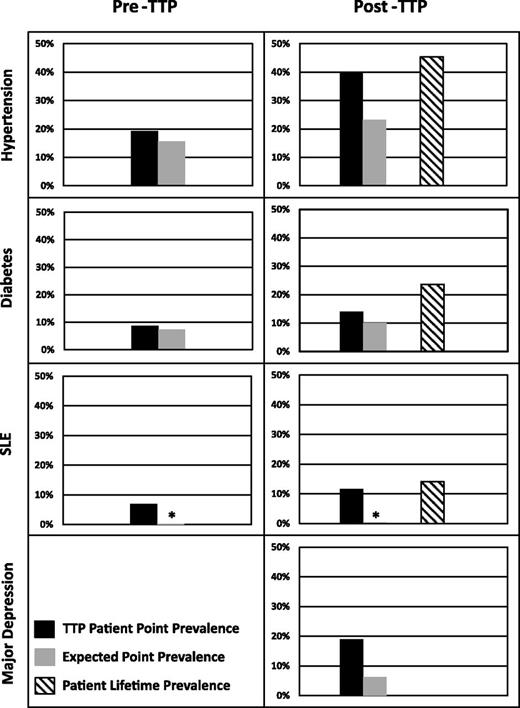
Hypertension and diabetes
At the time of their initial diagnosis of TTP, the prevalence of hypertension (19% vs 16%) and diabetes (9% vs 7%) among all 57 patients was not different from the expected values (Figure 3). In 2011-2012, 43 (93%) of the 46 surviving patients were evaluated for hypertension and diabetes (median follow-up, 7.0 years; range, 1.1 to 16.5 years); the prevalence of hypertension (40%) was significantly greater than the expected value (23%; P = .011); the prevalence of diabetes (14%) was not different (10%; P = .439). Among 55 patients with data following recovery (patients #29 and #36 were omitted; median follow-up, 5.8 years; range 0.5 to 16.7 years), the lifetime prevalence, including assessments throughout the entire follow-up period, was 45% for hypertension and 24% for diabetes (Figure 3).
Prevalence of hypertension, diabetes, SLE, and major depression following recovery from TTP. Black bars for pre-TTP data represent point prevalence for all 57 patients at the time of their initial diagnosis of TTP. Black bars for post-TTP data for hypertension, diabetes, and SLE represent point prevalence data for 43 (93%) of the 46 surviving patients who were assessed in 2011-2012, comparable to the 2-year cycles of NHANES point prevalence data. The black bar for major depression represents point prevalence data for 37 (80%) of the 46 surviving patients who were assessed in 2012. Gray bars represent expected prevalence based on the NHANES US reference population. Hatched bars represent lifetime prevalence from assessments over the entire follow-up period for 55 (96%) of the 57 surviving patients for whom post-TTP data were available. Lifetime prevalence proportions were hypertension (45%), diabetes (24%), and SLE (14%). Pre-TTP point prevalence of hypertension among patients (19%) was not different from the expected prevalence from the NHANES US reference population (16%; P = .442); post-TTP point prevalence among patients (40%) was greater than the expected prevalence of the NHANES US reference population (23%; P = .011). Both pre-TTP (9%) and post-TTP (14%) point prevalences of diabetes were not different from the expected prevalence of the NHANES US reference population (7%; P = .799; 10%; P = .439). Both pre-TTP (7%) and post-TTP (12%) point prevalences of SLE were greater than the expected prevalence of the NHANES US reference population (0.3%, indicated by the asterisk; P < .001). The post-TTP point prevalence of major depression (19%) was greater than the expected prevalence from the NHANES US reference population (6%; P = .005).
Prevalence of hypertension, diabetes, SLE, and major depression following recovery from TTP. Black bars for pre-TTP data represent point prevalence for all 57 patients at the time of their initial diagnosis of TTP. Black bars for post-TTP data for hypertension, diabetes, and SLE represent point prevalence data for 43 (93%) of the 46 surviving patients who were assessed in 2011-2012, comparable to the 2-year cycles of NHANES point prevalence data. The black bar for major depression represents point prevalence data for 37 (80%) of the 46 surviving patients who were assessed in 2012. Gray bars represent expected prevalence based on the NHANES US reference population. Hatched bars represent lifetime prevalence from assessments over the entire follow-up period for 55 (96%) of the 57 surviving patients for whom post-TTP data were available. Lifetime prevalence proportions were hypertension (45%), diabetes (24%), and SLE (14%). Pre-TTP point prevalence of hypertension among patients (19%) was not different from the expected prevalence from the NHANES US reference population (16%; P = .442); post-TTP point prevalence among patients (40%) was greater than the expected prevalence of the NHANES US reference population (23%; P = .011). Both pre-TTP (9%) and post-TTP (14%) point prevalences of diabetes were not different from the expected prevalence of the NHANES US reference population (7%; P = .799; 10%; P = .439). Both pre-TTP (7%) and post-TTP (12%) point prevalences of SLE were greater than the expected prevalence of the NHANES US reference population (0.3%, indicated by the asterisk; P < .001). The post-TTP point prevalence of major depression (19%) was greater than the expected prevalence from the NHANES US reference population (6%; P = .005).
SLE
Among the 57 survivors, 4 (7%) had been diagnosed with SLE before their initial diagnosis of TTP, a prevalence greater than the expected value (0.3%; P < .001). Four additional patients were diagnosed with SLE following their initial diagnosis of TTP. Two of the previously diagnosed and 1 of the subsequently diagnosed patients died during follow-up. Therefore, the prevalence of SLE at follow-up of the 43 patients in 2011-2012 was 12%, also greater than the expected value (0.3%; P < .001). The lifetime prevalence of SLE was 14% (Figure 3).
Depression
In 2012, 37 (80%) of 46 surviving patients were evaluated for current depressive symptoms by the PHQ-8 (median follow-up, 6.3 years; range 1.8 to 16.2 years); 7 (19%) had scores suggesting major depression, significantly greater than the expected value (6%; P = .005; Figure 3). At the time the PHQ-8 was administered, 2 of the 7 patients who had scores suggesting major depression and 8 of the other 30 patients were taking antidepressant medication. Among the 7 patients who had scores suggesting major depression, 2 had had stroke symptoms, and none had had seizures or coma; they required 8 to 37 PEX treatments (median, 18 PEX treatments) to achieve a remission; none had relapsed. Among the other 30 patients, 2 had had stroke symptoms, 5 had had seizures, and none had coma; they required 8 to 74 PEX treatments (median, 15 PEX treatments) to achieve a remission; 9 had relapsed. There were no differences between the 7 patients who had scores suggesting major depression and the other 30 patients regarding the severity of their TTP based on these observations.
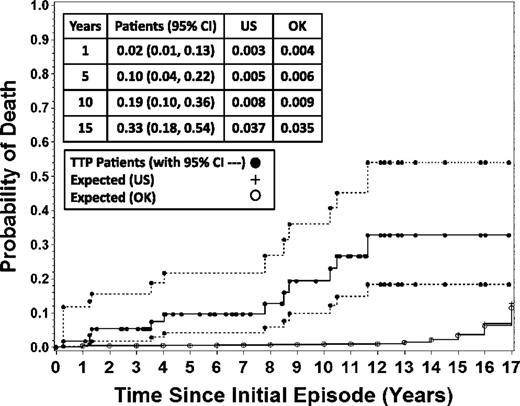
Death
With a median follow-up of 7.8 years (range, 0.3 to 17.1 years; through 2012), 11 (19%) of the 57 patients died, a proportion greater than expected proportions in the US and Oklahoma reference populations (Figure 4). All 11 patients died before their expected age of death (median difference, 30 years; range, 4 to 41 years; Table 1). Table 1 presents the data available for estimating causes of death. Patient 15 died of relapsed TTP. Patient 3 died of a myocardial infarction following recovery from a TTP relapse. In the other 9 patients, there was no evidence for TTP relapse at the time of their death. Among the 21 patients who have relapsed, 6 (29%) have died compared with 5 (14%) of 36 patients who have not relapsed (P = .296). Seven of the 11 patients who died had ADAMTS13 measurements during remission; 1 had activity <10%; 2 had activities of 11% and 14%; and 4 had values of 100% (Table 1). All 11 patients who died had 1 or more comorbidities (hypertension, diabetes, and/or SLE) which may have contributed to their death. When the three patients with SLE who died were excluded from the analysis, the probability of death remained significantly greater than the US and Oklahoma reference populations (data not shown).
Mortality of the 57 patients following recovery from TTP. The probability of patient death (solid circles) is compared with the expected probability based on age, race, and gender-specific rates from the reference United States (US; +) and Oklahoma (OK; open circles) populations obtained from the CDC. Broken lines indicate the 95% confidence intervals (CIs) around the patient mortality. The probability of patient death and 95% CIs as well as the population probability of death for the US and Oklahoma were calculated by using the Kaplan-Meier methods with point-wise limits. The data for the probability of patient death at 1, 5, 10, and 15 years after their initial episode of TTP, with 95% CIs and expected probability of death based on the US and Oklahoma reference populations are presented in the box.
Mortality of the 57 patients following recovery from TTP. The probability of patient death (solid circles) is compared with the expected probability based on age, race, and gender-specific rates from the reference United States (US; +) and Oklahoma (OK; open circles) populations obtained from the CDC. Broken lines indicate the 95% confidence intervals (CIs) around the patient mortality. The probability of patient death and 95% CIs as well as the population probability of death for the US and Oklahoma were calculated by using the Kaplan-Meier methods with point-wise limits. The data for the probability of patient death at 1, 5, 10, and 15 years after their initial episode of TTP, with 95% CIs and expected probability of death based on the US and Oklahoma reference populations are presented in the box.
Characteristics of the 11 patients who died following recovery from their initial episode of TTP
| Patient No. . | Date . | Age, y . | Expected age of death, y . | Clinical course, attributed cause of death . | |
|---|---|---|---|---|---|
| First TTP . | Death . | ||||
| 2 | 1996 | 2007 | 46 | 70 | SLE diagnosed during a TTP relapse 4 months after initial TTP. Continuous treatment with steroids and plaquenil for the following 11 years. Five hospitalizations for alcohol/drug abuse, pancreatitis, hypertension, diabetes. ADAMTS13 activity was 100% in 2004. Died in hospital: sepsis. |
| 3 | 1996 | 1998 | 59 | 80 | Sudden death during outpatient PEX to consolidate response for first relapse of TTP; platelet count 181 000/µL on day of death. Diabetes. Autopsy: acute myocardial infarction superimposed on previous infarction; no systemic microvascular thrombi. |
| 6 | 1997 | 2007 | 51 | 81 | Four relapses from 1997 to 2002. Liver cirrhosis with portal hypertension (biopsy, nonalcoholic steatohepatitis), liver transplant recommended. Hypertension, diabetes, chronic obstructive pulmonary disease (COPD). ADAMTS13 activity 100% 2 months before death. Died in nursing home. Death certificate: Cirrhosis of liver. |
| 7 | 1998 | 2001 | 51 | 78 | Two days after initial diagnosis of TTP, presenting clinical features attributed to streptococcal sepsis; PEX stopped. No relapse. Insulin-dependent diabetes since 1993 with episodes of ketoacidosis. Alcohol abuse. Died at home. Death certificate: Acute coronary insufficiency. |
| 9 | 1999 | 2009 | 82 | 86 | One relapse in 1999. Hypertension, Alzheimer’s disease, COPD on continuous nasal O2, myocardial infarction in 2008. ADAMTS13 activity 100% at 1 year before death. Died in nursing home. Death certificate: Cerebrovascular event. |
| 11 | 1999 | 2008 | 76 | 85 | Diabetes, hypertension, and heart failure. Died several years after admission to a nursing home. ADAMTS13 activity 100% 2 years before death. Death certificate: Cardiopulmonary failure. |
| 15 | 2000 | 2004 | 51 | 74 | No previous relapse. Hypertension. Acute myocardial infarction; coronary artery bypass grafting surgery; sudden death in hospital on sixth postop day (hematocrit 32%, platelet count 134 000/µL on second postop day; no subsequent laboratory data). ADAMTS13 14% (no inhibitor) 3 weeks before death. TTP not suspected until the day of death. Autopsy: systemic microvascular thrombi consistent with TTP. |
| 19 | 2000 | 2009 | 42 | 77 | Hypertension. Metastatic ovarian carcinoma, 2008; unresponsive to chemotherapy; ADAMTS13 11% (no inhibitor) 2006. Two relapses of TTP after diagnosis of metastatic carcinoma. Hospice care. Death certificate: Ovarian cancer. |
| 20 | 2001 | 2008 | 46 | 82 | Hypertension, diabetes. Ten hospitalizations for bipolar disorder with suicide risk during previous 20 years. ADAMTS13 activity <10% (no inhibitor) 6 months before death. Sudden death at home. Death certificate: Cardiac arrest. |
| 29 | 2003 | 2003 | 46 | 79 | Diagnosed with SLE in 1992. Sudden death at home. Death certificate: Cerebrovascular accident. |
| 34 | 2005 | 2006 | 41 | 82 | Diagnosed with SLE, scleroderma, 1994; jejunostomy for gastric paresis, 2002. Hospitalized for intestinal fistulas and recurrent sepsis for 13 of the 15 months she survived after her initial diagnosis of TTP. Died in hospital: intestinal hemorrhage. |
| Patient No. . | Date . | Age, y . | Expected age of death, y . | Clinical course, attributed cause of death . | |
|---|---|---|---|---|---|
| First TTP . | Death . | ||||
| 2 | 1996 | 2007 | 46 | 70 | SLE diagnosed during a TTP relapse 4 months after initial TTP. Continuous treatment with steroids and plaquenil for the following 11 years. Five hospitalizations for alcohol/drug abuse, pancreatitis, hypertension, diabetes. ADAMTS13 activity was 100% in 2004. Died in hospital: sepsis. |
| 3 | 1996 | 1998 | 59 | 80 | Sudden death during outpatient PEX to consolidate response for first relapse of TTP; platelet count 181 000/µL on day of death. Diabetes. Autopsy: acute myocardial infarction superimposed on previous infarction; no systemic microvascular thrombi. |
| 6 | 1997 | 2007 | 51 | 81 | Four relapses from 1997 to 2002. Liver cirrhosis with portal hypertension (biopsy, nonalcoholic steatohepatitis), liver transplant recommended. Hypertension, diabetes, chronic obstructive pulmonary disease (COPD). ADAMTS13 activity 100% 2 months before death. Died in nursing home. Death certificate: Cirrhosis of liver. |
| 7 | 1998 | 2001 | 51 | 78 | Two days after initial diagnosis of TTP, presenting clinical features attributed to streptococcal sepsis; PEX stopped. No relapse. Insulin-dependent diabetes since 1993 with episodes of ketoacidosis. Alcohol abuse. Died at home. Death certificate: Acute coronary insufficiency. |
| 9 | 1999 | 2009 | 82 | 86 | One relapse in 1999. Hypertension, Alzheimer’s disease, COPD on continuous nasal O2, myocardial infarction in 2008. ADAMTS13 activity 100% at 1 year before death. Died in nursing home. Death certificate: Cerebrovascular event. |
| 11 | 1999 | 2008 | 76 | 85 | Diabetes, hypertension, and heart failure. Died several years after admission to a nursing home. ADAMTS13 activity 100% 2 years before death. Death certificate: Cardiopulmonary failure. |
| 15 | 2000 | 2004 | 51 | 74 | No previous relapse. Hypertension. Acute myocardial infarction; coronary artery bypass grafting surgery; sudden death in hospital on sixth postop day (hematocrit 32%, platelet count 134 000/µL on second postop day; no subsequent laboratory data). ADAMTS13 14% (no inhibitor) 3 weeks before death. TTP not suspected until the day of death. Autopsy: systemic microvascular thrombi consistent with TTP. |
| 19 | 2000 | 2009 | 42 | 77 | Hypertension. Metastatic ovarian carcinoma, 2008; unresponsive to chemotherapy; ADAMTS13 11% (no inhibitor) 2006. Two relapses of TTP after diagnosis of metastatic carcinoma. Hospice care. Death certificate: Ovarian cancer. |
| 20 | 2001 | 2008 | 46 | 82 | Hypertension, diabetes. Ten hospitalizations for bipolar disorder with suicide risk during previous 20 years. ADAMTS13 activity <10% (no inhibitor) 6 months before death. Sudden death at home. Death certificate: Cardiac arrest. |
| 29 | 2003 | 2003 | 46 | 79 | Diagnosed with SLE in 1992. Sudden death at home. Death certificate: Cerebrovascular accident. |
| 34 | 2005 | 2006 | 41 | 82 | Diagnosed with SLE, scleroderma, 1994; jejunostomy for gastric paresis, 2002. Hospitalized for intestinal fistulas and recurrent sepsis for 13 of the 15 months she survived after her initial diagnosis of TTP. Died in hospital: intestinal hemorrhage. |
Individual data for each of the 11 patients who have died following recovery from their initial episode of TTP. Patients’ numbers represent the sequence of their enrollment in the Registry, as designated in supplemental Table S1. Median difference between the actual age at death and the expected age at death, calculated from the time of their initial diagnosis of TTP, was 30 years (range, 4 to 41 years).
Discussion
Since the beginning of the era of effective treatment for patients with TTP, reports of survival have focused on recovery from acute episodes.3,5 Although recovery from acute episodes typically appears to be complete, long-term survival data for this group compared with population data has not been previously described. Our cohort of 57 consecutive patients who had TTP associated with severe acquired ADAMTS13 deficiency and who survived their initial acute episode provided the opportunity to document long-term outcomes. Following recovery, these patients had an increased prevalence of hypertension and major depression. Eleven (19%) have died, all before their predicted age of death, a proportion greater than expected for the US and Oklahoma reference populations. We have considered 4 possible explanations for the increased morbidities and mortality.
First, death may be related to relapses of TTP. However death with a relapse is uncommon since relapses of TTP are typically recognized promptly and treated effectively. Among our 57 patients, 21 have had 1 to 4 relapses. Only 1 patient has died of a relapse, which occurred following cardiac surgery and was diagnosed only at autopsy. One other patient died of a myocardial infarction during a final PEX procedure following successful treatment of a TTP relapse; she had no evidence for TTP at autopsy. Although there was no evidence for a TTP relapse in the other 9 patients who died, an unrecognized relapse cannot be excluded.
Second, ADAMTS13 deficiency during clinical remission may be a risk factor for cardiovascular and cerebrovascular disease. Studies in mice have suggested a protective, antiinflammatory role for ADAMTS13 in cardiac injury.18,19 These experimental data suggest that ADAMTS13 deficiency during remission may be clinically important. However the natural history of ADAMTS13 activity during remission following recovery from TTP is poorly understood. Whether the occurrence of severe ADAMTS13 deficiency during remission is associated with increased risk for relapse could not be determined from our data.
Third, ischemia caused by systemic microvascular thromboses during acute TTP episodes may cause persistent organ damage. We and others have previously documented persistent minor cognitive abnormalities in patients who have recovered from TTP.10,20 Case reports have suggested that persistent kidney and cardiac abnormalities may also occur and contribute to poor health outcomes.21-23 However, we did not document chronic kidney injury with measurements of GFR and microalbuminuria. We have not measured cardiac function following recovery.
Fourth, increased mortality following recovery from TTP may be related to risk factors for poor health outcomes that occur in people who have TTP associated with acquired severe ADAMTS13 deficiency. These patients have significant race and gender disparities with an increased relative frequency of blacks and women, similar to the demographics for SLE.12,24 Eight (14%) of the 57 survivors were diagnosed with SLE before or after their initial diagnosis of TTP; 3 of these 8 patients have died. An increased frequency of autoimmune disorders among patients with TTP associated with acquired severe ADAMTS13 deficiency has been previously reported.25,26 The predominant age, race, and gender of patients who develop TTP are all associated with a greater prevalence of major depression27 and the prevalence of major depression was increased among our patients who survived their initial episode of TTP. Depression erodes quality of life and productivity and is associated with an increased risk for death.28,29 Depression has a reciprocal relationship with obesity; depression is predictive for development of obesity and obesity increases the risk for depression.30 The prevalence of obesity, particularly morbid obesity (BMI ≥40 kg/m2), was significantly increased among our patients at the time of their initial diagnosis of TTP. Obesity is a principal risk factor for cardiovascular disease, including hypertension,31 and is associated with increased all-cause mortality.17,31-33 The prevalence of hypertension was increased among our patients who survived their initial episode of TTP. Even though we attempted to control for the age, race, gender, and BMI differences of our patients, these demographic factors as well as additional unknown factors may have contributed to the observed poor health outcomes of our patients.
This study is limited by the small number of patients, an inevitable issue for an uncommon disorder, which prevented analysis for possible associations among risk factors for poor health and death. Although we adjusted for demographic variables, the small number of patients also did not allow determination that TTP was independently associated with the morbidities. The cross-sectional analysis design, which uses period prevalence, was selected to allow comparison with existing national data. One limitation of this study design is that it does not identify occurrence across a longer period of time, so some patients may have experienced an outcome such as depression that was not present at the time of our study. Therefore, our data may underestimate the prevalence of these morbidities. However the small number of patients allowed nearly complete long-term follow-up of almost all patients with detailed analyses of individual patient data. We believe that our comprehensive data on consecutive unselected patients for up to 16 years following recovery from an initial episode provide a unique perspective for understanding the clinical course of TTP.
Recognition of increased morbidity and mortality among patients following recovery suggests that TTP may, in some patients, be more of a chronic disorder rather than a disorder of acute episodes and complete recovery. These observations suggest that recovery from an acute episode of TTP is not a conclusion of care, but rather the beginning of a requirement for long-term health care. The occurrence of obesity, hypertension, depression, and SLE in these patients highlights issues of public health and primary care in addition to the need for investigation to understand the continuing health problems associated with TTP survivorship.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by the Hematology Research Fund of the University of Oklahoma Health Sciences Center. J.A.K.H. and B.L. were supported by a grant from the Swiss National Science Foundation (32003B-124892). D.R.T. was supported by a grant from the National Institutes of Health (1U01HL72283).
Authorship
Contribution: J.N.G., S.K.V., and D.R.T. designed the research; C.C.D., J.A.R., L.H.S., J.J.P., J.N.G., J.A.K.H., and B.L. collected data; L.H.S., J.J.P., J.A.K.H., B.L., D.R.T., S.K.V., and J.N.G. analyzed and interpreted data; J.A.R. and S.K.V. performed statistical analysis; J.N.G. wrote the manuscript; and C.C.D., J.A.R., L.H.S., J.J.P., J.A.K.H., B.L., D.R.T., S.K.V., and J.N.G. edited the manuscript.
Conflict-of-interest disclosure: B.L., J.A.K.H., and J.N.G. are consultants for Baxter, Inc. for the development of rADAMTS13 as a potential treatment of TTP. J.N.G. is a consultant for Alexion, Inc. for eculizumab as treatment of aHUS. The remaining authors declare no competing financial interests.
Correspondence: James N. George, Department of Biostatistics and Epidemiology, College of Public Health, The University of Oklahoma Health Sciences Center, Room CHB 237, PO Box 26901, Oklahoma City, OK 73126-0901; e-mail: james-george@ouhsc.edu.
References
Author notes
C.C.D. and J.A.R. contributed equally to this manuscript.