Abstract
Genetic analysis of hematologic malignancies over the past 5 years has revealed abundant mutations in epigenetic regulators in all classes of disorders. Here, we summarize the observations made within our review series on the role of epigenetics in hematology. We highlight the clinical implications of mutations in epigenetic regulators and outline what we envision are some of the major areas that merit future research. Recent findings may have immediate prognostic value, but also offer new targets for drug development. However, the pleiotropic action of these regulators indicates caution is warranted and argues for investment in understanding of their underlying mechanisms of action as we proceed to exploit these findings for the benefit of patients.
In this issue, we present the last of our series of reviews surveying epigenetics in hematology. We started with an overview of the foundations of epigenetics with respect to hematology and have explored the clinical relevance of epigenetics for each of the major classes of hematologic malignancies (Table 1 1-5 ). Here, we bring together observations from all of these reviews to highlight some of the major areas that merit more research and discuss areas of future study. We hope that these observations collectively will challenge and inspire new directions of investigation in this burgeoning area and will have both basic and clinical impact.
Reviews in this series
| Review . | Authors and affiliations . | Reference . |
|---|---|---|
| The role of chromatin modifiers in normal and malignant hematopoiesis | Jill Butler and Sharon Dent The University of Texas M. D. Anderson Cancer Center Science Park | 1 |
| Mechanisms of epigenetic deregulation in lymphoid neoplasms | Yanwen Jiang, Katerina Hatzi, and Rita Shaknovich Weill Cornell Medical Center | 2 |
| Mutations in epigenetic modifiers in the pathogenesis and therapy of AML | Omar Abdel-Wahab and Ross Levine Memorial Sloan-Kettering Cancer Center | 3 |
| The myelodysplastic syndrome as a prototypical epigenetic disease | Jean-Pierre Issa Fels Institute, Temple University | 4 |
| Epigenetic mechanisms and MLL | Tobias Neff and Scott Armstrong University of Colorado and Memorial Sloan-Kettering Cancer Center | 5 |
| Review . | Authors and affiliations . | Reference . |
|---|---|---|
| The role of chromatin modifiers in normal and malignant hematopoiesis | Jill Butler and Sharon Dent The University of Texas M. D. Anderson Cancer Center Science Park | 1 |
| Mechanisms of epigenetic deregulation in lymphoid neoplasms | Yanwen Jiang, Katerina Hatzi, and Rita Shaknovich Weill Cornell Medical Center | 2 |
| Mutations in epigenetic modifiers in the pathogenesis and therapy of AML | Omar Abdel-Wahab and Ross Levine Memorial Sloan-Kettering Cancer Center | 3 |
| The myelodysplastic syndrome as a prototypical epigenetic disease | Jean-Pierre Issa Fels Institute, Temple University | 4 |
| Epigenetic mechanisms and MLL | Tobias Neff and Scott Armstrong University of Colorado and Memorial Sloan-Kettering Cancer Center | 5 |
Overview
The earliest studies of molecular biology revealed the fundamental principles of gene regulation, including how the presence or absence, or modification, of transcription factors controls gene expression. From electron micrographs of bacterial chromosomes, we learned that DNA is highly organized through interaction with proteins, but it took several more decades before the histone “code” began to be elucidated. Through a great deal of basic research, we now know that histones keep DNA organized and compact, but also that specific histone modifications dramatically affect the accessibility of the DNA to factors that then enable (or inhibit) gene expression. Through fundamental studies using model organisms, the broader role of the enzymes that modify histones has begun to be elucidated, forming the foundation of the field of epigenetics.
Similarly, the importance of covalent modification of DNA by methylation was demonstrated early on by the recognition that the activity of restriction enzymes was altered by DNA methylation, a component of bacterial pathogen defense. But several more decades passed before we began to understand that there was also a “code” to the placement of DNA methylation in mammals,6 and that low levels of promoter methylation were associated with gene expression. Now the further modification of cytosine methylation to hydroxymethylation7 and related variants8,9 has been identified, the functions of which have yet to be fully elucidated.
Broadly speaking, both histone modifications and covalent modification of cytosine residues in DNA are referred to as “epigenetic” changes. As we defined in the introduction to this series,10 the term “epigenetic” refers to any heritable change that impacts cellular phenotype or physiology that does not occur at the level of alterations in the DNA sequence. Included in this grouping as well are the noncoding RNAs and microRNAs (miRNAs) that are now understood to have a major impact on chromosome structure and gene expression.
With the advent of sequencing of cancer genomes over the past 5 years, we have seen the extent to which mutations in the genes encoding enzymes responsible for histone and DNA modification can lead to disease (Table 2 11-42 ). Nowhere has this been more evident than within hematology. In their review, “The role of chromatin modifiers in normal and malignant hematopoiesis,”1 Butler and Dent review epigenetic regulatory mechanisms and describe how hematologic malignancies frequently show disruption in genes encoding chromatin-modifying enzymes as well as altered enzyme function through gain or loss of conserved domains that affects both histone and nonhistone substrates. They discuss how leukemia-specific fusion proteins formed via chromosomal translocations lead to altered localization of histone-modifying enzymes to inappropriate targets. However, because there are many targets that are different between the “normal” and altered states, we do not always know which are the most important changes.
Epigenetic regulators mutated in hematologic disease
| . | Molecule . | Diseases associated . | References . |
|---|---|---|---|
| Polycomb-repressive complex | EZH2 | FL, DLBCL, T-ALL, PBML, MDS, MPN, MF, AML | 11,,,,,,,-19 |
| SUZ12 | T-ALL | 16 | |
| EED | T-ALL | 16 | |
| ASXL1 | MDS, AML, CML | 19,20 | |
| Trithorax complex | MLL1 | B-ALL, T-ALL | |
| MLL2 | FL, DLBCL | 11,13,21 | |
| MLL rearrangements | ALL, AML | 22 | |
| Histone demethylase | UTX | MM | 23 |
| JMJD2C | PMBL, HL | 24 | |
| KDM2B | DLBCL | 21 | |
| Histone acetylation | CREBBP | DLBCL, FL | 13,25 |
| EP300 | DLBCL | 25,26 | |
| Histone methylation | MMSET | MM | 27 |
| Chromatin remodeling | ARID1A | Pediatric B-CLL, CLL | 28 |
| CHD2 | B-CLL | 29 | |
| DNA modification | DNMT3A | AML, MDS, ETP-ALL, AITL, PTCL, MF, CMML, MPN | 30,,-33,35 |
| TET2 | AML, MDS, MPN, MF, DLBCL, FL, AITL, PTL | 32,36,,-39 | |
| Other | IDH1/2 | MDS, AML, ETP-ALL | 34,38,40,-42 |
| HIST1HC | DLBCL | 11 |
| . | Molecule . | Diseases associated . | References . |
|---|---|---|---|
| Polycomb-repressive complex | EZH2 | FL, DLBCL, T-ALL, PBML, MDS, MPN, MF, AML | 11,,,,,,,-19 |
| SUZ12 | T-ALL | 16 | |
| EED | T-ALL | 16 | |
| ASXL1 | MDS, AML, CML | 19,20 | |
| Trithorax complex | MLL1 | B-ALL, T-ALL | |
| MLL2 | FL, DLBCL | 11,13,21 | |
| MLL rearrangements | ALL, AML | 22 | |
| Histone demethylase | UTX | MM | 23 |
| JMJD2C | PMBL, HL | 24 | |
| KDM2B | DLBCL | 21 | |
| Histone acetylation | CREBBP | DLBCL, FL | 13,25 |
| EP300 | DLBCL | 25,26 | |
| Histone methylation | MMSET | MM | 27 |
| Chromatin remodeling | ARID1A | Pediatric B-CLL, CLL | 28 |
| CHD2 | B-CLL | 29 | |
| DNA modification | DNMT3A | AML, MDS, ETP-ALL, AITL, PTCL, MF, CMML, MPN | 30,,-33,35 |
| TET2 | AML, MDS, MPN, MF, DLBCL, FL, AITL, PTL | 32,36,,-39 | |
| Other | IDH1/2 | MDS, AML, ETP-ALL | 34,38,40,-42 |
| HIST1HC | DLBCL | 11 |
AITL, angioimmunoblastic T-cell lymphoma; B-ALL, B-cell acute lymphoid leukemia; DLBCL, diffuse lymphoblastic B-cell lymphoma; ETP-ALL, early-T-precursor acute lymphoid leukemia; FL, follicular lymphoma; HL, Hodgkin’s lymphoma; MDS, myelodysplastic syndrome; MF, myelofibrosis; MM, multiple myeloma; PBML, primary mediastinal lymphoma; PTCL, peripheral T-cell lymphoma not otherwise specified; T-ALL, T-cell acute lymphoblastic leukemia.
We highlight here the regulators known to be mutated in a high frequency of the indicated diseases–please see individual disease-specific reviews for details and references therein. Many have not yet been unequivocally shown to be causal, but their repetitive occurrence in these diseases implicates them.
In parallel, DNA methylation variation in cancers has been analyzed independent of genetic alterations. Aberrant DNA methylation patterns are a hallmark of many hematologic as well as solid tumors. However, as Jiang, Hatzi, and Shaknovich remind us in their review, “Mechanisms of epigenetic deregulation in lymphoid neoplasms,”2 we have yet to demonstrate exactly how a deregulated epigenome leads to development of hematopoietic malignancies. Part of the challenge for unraveling the cause from effect is the sheer number of epigenetic changes that can be seen with new high-throughout-sequencing technologies. It is imperative that our next phase of work defines which specific epigenetic changes drive hematopoietic malignancies, and whether these alterations shift gene expression or other aspects of chromosome function in generating and propagating the tumor cells. Shaknovich and colleagues point out that we will need “a new generation of computer-savvy biologists … to provide solutions to the challenging data analysis. Until then we are only stealing small glimpses into the nature of epigenomic regulation.”2
Further complicating analysis, the appropriate reference epigenome is not always clear. As Issa warns in his review, “The myelodysplastic syndrome as a prototypical epigenetic disease,”4 “It is important but somewhat tricky to tease out epigenetic changes that are truly abnormal from those that simply reflect the differentiation state of the cells under study.” Furthermore, because changes in epigenetic regulation, by definition, can have pleiotropic effects, “even more difficult is the task of separating driver events from passenger events that arise as a function of time/neoplasia.”4 In this regard, it will be important in the future to compare the epigenetic changes found in cancer stem cells with those of normal hematopoietic stem cells, as well as to more broadly understand the molecular heterogeneity and clonal evolution occurring in the malignant populations.
Analyses of broad epigenetic differences are now converging with identification of genetic lesions. But we still do not understand the relationship between a genetic mutation in an epigenetic regulator and an aberrant methylation or histone-binding pattern in the malignant cells. Exactly how inactivating mutations such as those found in DNMT3A, TET2, IDH1/2, and ASXL1 disrupt the patterns of DNA cytosine modifications and consequent gene expression is an active area of current research. Nevertheless, understanding the association of mutations in these epigenetic regulators with disease outcome may lead to their use as biomarkers with prognostic value. In their review, “Mutations in epigenetic modifiers in the pathogenesis and therapy of acute myeloid leukemia,”3 Abdel-Wahab and Levine argued for the incorporation of mutational testing for DNMT3A, TET2, IDH1/2, and ASXL1 for patients with acute myeloid leukemia (AML) to provide risk stratification and biomarkers for detection of minimal residual disease. Furthermore, recent data suggest that mutations in particular epigenetic regulators (DNMT3A, TET2, Cohesins) are founding genetic lesions, thus would be found in the cancer stem cell population.43 Such lesions should be the most important targets for future drug development.
We argue that with deep mechanistic understanding of how the genetic lesions lead to malignancy, targeted therapies may be able to be developed as exemplified mixed lineage leukemia (MLL)-driven leukemias. As Neff and Armstrong wrote in their review, “Epigenetic mechanisms and mixed lineage leukemia,”5 MLL-expressing leukemias are the quintessential example of leukemias driven by epigenetic mechanisms because all members of the MLL family are histone methyltransferases that work with cofactor proteins to catalyze the addition of a methyl group to lysine 4 on histone H3. New drugs that interfere with MLL’s ability to bind to other members of higher-order protein complexes (eg, menin), those that block the activity of proteins required for MLL-induced transformation (eg, DOT1L), and those that read the histone code (eg, BRD4) hold great promise as novel approaches to these generally aggressive diseases. Understanding whether MLL fusion proteins exert their effects solely through modulation of histone modifications, or whether they have any effects similar to those of the inactivating gene mutations found in myeloid leukemias, is also an area of future focus.
Major questions and areas for development
The reviews in this series survey the state of the field with respect to epigenetics and hematologic malignancies. Here, we point out some gaps in knowledge that should be addressed both clinically and with basic research over the coming years with a view to developing new therapeutic approaches to target these “epigenetic” malignancies.
What is the role of noncoding RNAs?
Noncoding RNAs are increasingly being implicated in epigenetic regulation, but we currently understand their role poorly. Although many researchers were taught that the RNAs that ran very fast on gels were “small, unimportant RNA species,” we now recognize them as miRNAs, central to regulation of translation and protein function. Their overall importance for leukemias is suggested from the findings that miRNAs regulate many of the proteins that mediate epigenetic alterations and that their expression profiles can be used to accurately classify leukemias.44 Similarly, long noncoding RNAs are now being recognized as potentially enormously important. Noncoding RNAs may interact with the histone-modifying machinery.45 Moreover, in plants, noncoding RNAs are critically important for directing DNA methyltransferases to their targets. We currently have almost no understanding of how the de novo DNA methyltransferases DNMT3A and DNMT3B reach their targets, and it is intriguing to postulate that noncoding RNAs could play such a role.46 Current dogma states that human DNA methylation machinery acts very differently from its counterpart in plants, but we wonder whether more parallels actually exist. Do noncoding RNAs direct the DNA methyltransferase enzymes to their sites of action? Might they have a similar role in bringing the TET enzymes to specific DNA regions? As more cancer genomes undergo whole-genome sequencing, we may identify recurring mutations in putative noncoding RNAs.
Study of long noncoding RNAs presents unique challenges in associating them with specific functions as well as identifying where in the genome they act. Although mouse models have been of great value for protein-coding genes, long noncoding RNAs are thought to be less conserved among species, so mouse models may not be as useful for functional validation of human malignancy-associated noncoding RNA species. As occurred when interest in miRNAs surged, new technologies will need to be developed to fully explore the role of long noncoding RNAs. Clearly, their prevalence as well as some early functional data suggest their importance.47,48 Specific RNA-protein interactions also need to be identified. Such studies have the potential to elucidate fundamental biological mechanisms as well as lead to new therapeutic targets.
How do mutations in DNA methylation regulators promote leukemia?
Although the existence of 5-hydroxymethylcytosine in mammalian DNA was known from chromatography experiments performed in the early 1970s,49 its functional importance was not recognized until the catalytic activity of the TET enzymes was defined in the late 2000s, as that which catalyzes the formation of 5-hydroxymethyl-, formyl-, and carboxyl-cytosine from 5-methylcytosine.7-9 The recognition of genetic mutations in genes encoding proteins critical for the processing of 5-methylcytosine, DNMT3A, TET2, IDH1, IDH2, and possibly others, commonly within hematopoietic malignancies,30,31,36,37,50 as well as aberrant DNMT3B transcription51,52 and translocation of TET1 in MLL-rearranged leukemias, argues for a prominent role for these derivatized cytosine DNA bases in hematopoietic cell differentiation53 and development of malignancies.
Beyond the general paradigm that mutation of these regulators of DNA methylation impedes cellular differentiation, we do not understand how they lead directly to malignancy. From a biochemical standpoint, TET protein activity appears to lead to DNA demethylation, therefore we might assume that mutations in TET proteins and DNMT3A would oppose each other. Curiously, however, mutation of either DNMT3A, or TET2, leads to similar hematopoietic malignancies, namely AML, myelodysplastic/myeloproliferative diseases, and lymphomas. Moreover, mutations of DNMT3A and TET2 can be found in the same malignant clones, for example in AML43,54 as well as in T-cell lymphomas,32 suggesting they are neither antagonistic nor redundant mutations. IDH mutations have been thought to act at least in part by generation of an oncometabolite that inhibits TET2,50,55 and correspondingly, malignancies with both DNMT3A and IDH mutations are observed.54
Alterations in functions of such fundamental regulators might be expected to produce either random changes in DNA methylation, or profound genome-wide epigenetic dysregulation. Although DNA methylation patterns are indeed altered in the relevant malignancies, they are more limited than expected and they do not always correlate well with changes in gene expression that can be easily linked to disease development.30,50 However, most current studies have characterized methylation changes using technologies that are heavily biased toward interrogating CpG islands, which potentially miss important alterations in other genomic regions. The use of techniques that measure cytosine methylation and hydroxymethylation across the entire genome at single-base resolution should help resolve this conundrum.
It is also possible that the lack of large-scale changes in methyl cytosine suggests that the mutant proteins alter chromosome function via alternative mechanisms, for example, possibly through interactions with proteins involved in genome stability or telomeres.56 Deeper investigation of the methylation changes found in the context of mutant proteins, as well as understanding their specific protein-protein interactions, will be critical to understanding how they contribute to malignancy development. A full understanding of the functions of these proteins should also elucidate why mutations in DNMT3A and TET2 are genetically congruent rather than oppositional. Overall, improved understanding of these mechanisms may lead to better prognostic value and possible manipulation of these pathways for therapeutic ends.
Pathologic consequences of aberrant DNA methylation
Abberant DNA methylation has been observed in a number of malignancies separate from the identification of mutations in genes involved in epigenetic regulation. In hematologic malignancies, as well as in solid tumors, both increases and decreases in DNA methylation are observed. Broadly, increases in methylation are often associated with CpG islands and are thought to induce repression of tumor-suppressor genes. Genome-wide hypomethylation may also have pathologic consequences that have not yet been fully considered. Hypomethylation may make it more difficult to shut down regulators of self-renewal, perpetuating a stem cell state and inhibiting differentiation.53 We need more studies both in mouse models and in human samples that start with homogeneous cell populations, analyze progenitors and progeny, and examine DNA methylation and gene expression changes in tandem.
Confounding some analyses is the inability to distinguish between 5-methycytosine and 5-hydroxymethylcytosine which may have distinct roles in regulating gene expression and outcomes. We should reexamine what fraction of DNA methylation changes are actually due to 5-hydroxymethylation (or other derivatives) in both mouse models and human samples.
We still understand only poorly the specific implications of aberrant methylation. To what extent is the pathology driven by the dysregulation of a small specific set of critical genes, or more broadly, many events that make the cellular environment more conducive to enhancing the impact of secondary events–more like a drought sets the stage for a forest fire. Most of the technologies to address these questions are currently in place and the answers should become more clear in the next few years.
The true mechanism of action of the hypomethylating agents
Because there is significant interest in the pharmaceutical industry in generating drugs that inhibit DNA methylation enzymes more specifically, we argue that defining the mechanism of action of the so-called hypomethylating agents is critical to address. Because 5-azacitidine is thought to work by forcing methylation loss, the success of the drug in the clinic has been attributed to reversing hypermethylation of tumor suppressor genes within the malignant clone. However, some genomic loci actually gain DNA methylation after drug treatment, suggesting that a much more complicated series of reactions is probably at work. We have little insight into how these drugs impact DNA methylation at specific loci, and how this affects the distribution of 5-hydroxymethylcytosine. We submit that the molecular mechanism(s) by which 5-azacitidine works remains to be elucidated fully.
Moreover, clinical studies have shown a survival advantage for 5-azacitidine that has not yet been replicated for decitabine.57-59 Is the observed survival advantage simply a function of clinical trial designs, or could it be a function of drug chemistry? 5-azacitidine is a nucleoside base attached to ribose sugar, whereas decitabine has the same chemical ring, but is attached to deoxyribose. As expected, decitabine is primarily incorporated into DNA, but 5-azacitidine is incorporated into RNA as well as DNA.60 Indeed, Lyko and colleagues have shown that 5-azacitidine is incorporated into RNA species and results in hypomethylation of transfer RNA.61 Although dozens of covalently modified RNA species are recognized currently, studying how 5-azacitidine changes RNA species is technically challenging, and we suggest this area is ripe for reexamination. 5-azacitidine–modified RNA could have an even greater impact than in DNA. Again, understanding how this important class of drugs works is imperative as we begin to stratify and treat patients partly on the basis of mutations in genes encoding DNA-modifying enzymes, and seek to develop new more targeted drugs.
Answers to these questions may come from reexamination of the predominant biochemical interactions between 5-azacitidine and decitabine in normal and malignant cells. In addition, alterations of DNA methylation and RNA metabolism before, during, and after 5-azacitidine treatment in normal and malignant cells will be of value.
Exploiting disruption in histone modifications for therapeutic gain
The identification of DOT1L as a histone K79 methyltransferase with particular functional importance in MLL-driven leukemias brought with it the potential for designing specific inhibitors. DOT1L inhibition has proven to be remarkably successful to date,62 raising the potential for another successful example of targeted therapy. It is satisfying that the first drug with specific epigenetic effects will be applied to some of the most aggressive leukemias we dare to treat. Because of the tight link between histone and DNA modifications, it may also be possible to manipulate one to effect change in the other; basic research that illuminates the interplay between histone and DNA modifications could have implications for novel treatments. Considering the large number of proteins involved in histone modification, we expect that additional critical components are waiting to be identified that may serve as new drug targets.
Mutations in cohesin complex genes
Recent high-throughput-sequencing efforts have also uncovered rare mutations in several genes encoding proteins of the cohesion complex implicated as founding clone mutations.43 Their presence in parallel with the epigenetic regulators suggests their role in the higher order control of gene expression, perhaps somehow dove-tailing with the epigenetic regulators with regard to the development of epigenetic malignancy. Of note, DNMT3B has been reported to be part of the condensin complex,63 potentially linking higher-order chromosome structure with epigenetic regulation. The fact that it has been difficult to define large-scale changes in cytosine modifications in AMLs with DNMT3A mutations may imply that the catalytic function is not the only important aspect of the molecule. Might hematopoietic malignancies be driven by altered chromosome cohesion/condensation mediated by disrupted DNMT3 proteins? What other biochemical functions are controlled by DNA methyltransferase and/or TET enzymes? Both protein families have large N-terminal regions that mediate protein-protein interactions and C-terminal catalytic domains. There may be key functions in their N termini that could be uncovered by deep biochemical analyses of their proteins and of potential interactions. In addition, mouse models should be exploited to understand the role of the highly conserved cohesion family members in hematopoiesis.
Pediatric vs adult tumorigenesis
Comparison of pediatric hematopoietic neoplasms and their adult counterparts presents several intriguing questions:
In general, why do pediatric diseases with a related adult counterpart frequently have fewer and different mutations? We suspect this reflects a different epigenetic state of hematopoietic tissues from young individuals that somehow changes during transition to adulthood. Much work needs to be invested in understanding the epigenetics of this developmental shift. A better characterization of the key epigenetic regulators at play during normal development would be one place to start.
Why is the genetic mutation spectrum so different between adult and pediatric patients with similar diseases? For example, DNMT3A mutations are found frequently in adult AMLs, but almost never in pediatric cases. Understanding how the functions of this and other epigenetic regulators change with developmental age may elucidate this question.
Are these mutational spectrum differences purely a function of how long it takes certain mutations to exert their effects, or are there unique biologic drivers in pediatric vs adult diseases? Deep sequencing of normal samples from different ages may reveal the prevalence of occult mutations, lending insight into this question.
We suggest that a deeper understanding of these differences between pediatric and adult malignancies could yield clues as to how to treat patients of all ages more effectively.
Aging and increased malignancy
What aspects of aging contribute to the increased malignancy rate? Are there epigenetic changes that occur with age that are independent of mutations that contribute to the increased prevalence of malignancies? Such changes may affect cellular fitness, enabling the impact of preexisting mutations to be manifest.64 It is likely that many aging individuals harbor mutations in some of these epigenetic regulators,65 but some secondary environmental features foster their molecular impact. A better understanding of these epigenetic/environmental factors might even allow patients means of reversing, at least in part, the effects of aging. To start, we need a complete picture of how epigenetic regulators change with age, and how the epigenetic modifications change with age with humans, such as has been initiated in the mouse.66 We also need deep analysis of normal aging samples to better understand the prevalence of mutations and perhaps to conduct prospective studies to view the long-term significance of early mutations. Distinguishing causation from correlation with aging studies can be challenging because of so many pleotropic alterations. Nevertheless, as consistent patterns emerge, their relevance can be tested experimentally in mouse models using both genetic and biochemical approaches.
Prevalence of epigenetic mutations in hematologic malignancies
Is the prevalence of mutations in epigenetic regulators greater within hematologic malignancies? The apparently high frequency may reflect the dynamic nature of the hematopoietic system, and the fact that the constant turnover of the blood represents ongoing “developmental biology” to a greater degree than other regenerating tissues. Nevertheless, we may see additional epigenetic regulators emerging from The Cancer Genome Atlas project. Alternatively, other mechanisms of “knocking out” such regulators such as silencing via noncoding RNAs may be more prevalent in other tissues. As more data from the The Cancer Genome Atlas and similar projects emerge, the data can be exploited to address some of these questions.
Implications for pharmacologic interventions
Our current ability to define the global genetic and epigenetic changes present within individual tumors brings with it the promise that we will be able to classify our patients’ diseases and predict responsiveness to drug treatments more accurately. Some groups have correlated particular treatment responses with singular gene mutations,67 but whether a more comprehensive genetic analysis of the samples would skew the results is not known. Although some studies have already performed large-scale genetic analyses on clinically derived samples and predicted associated drug sensitivities,54 no one has combined these yet with epigenetic studies. Therefore, our hypothesis that combination genetic and epigenetic profiling will be superior to genetic studies alone is not yet confirmed experimentally.
Conclusions
In the past 3 years, the enormous clinical importance of correct epigenetic regulation has become increasingly evident. From a basic science perspective, this is an enormously exciting time because the patient data, more than anything else, illuminate the relevance of these protein complexes. From a clinical perspective, the new data should lead to improvements in approaches to treatment. In the short run, we may have improved patient stratification that will guide choices of existing treatments.68 In the long run, we should be able to devise new pharmacologic approaches to intervention, and the MLL-driven leukemias may be the first example where these clinical successes will be seen.
Returning to a cosmologic analogy with which we started this review series,10 we posit that epigenetic regulation is the dark matter of the universe (Figure 1). The transcription factors and signaling molecules that have been the focus of the previous decades of malignant hematology are the concrete celestial bodies that we can easily see and measure. In contrast, epigenetic regulation is biology’s dark energy–it is everywhere, making up an estimated 71% of the universe, not easy to see and requiring exquisitely precise measurements to detect. In a similar way, epigenetic alterations are ubiquitous in cells, at the heart of all cellular processes, connected in ways we still do not understand, and requiring ever more ingenious methodologies to measure properly. We look forward to the day when we can present a “standard model” for hematology that unites genetic and epigenetic principles to explain hematopoietic cell differentiation, both normal and diseased.
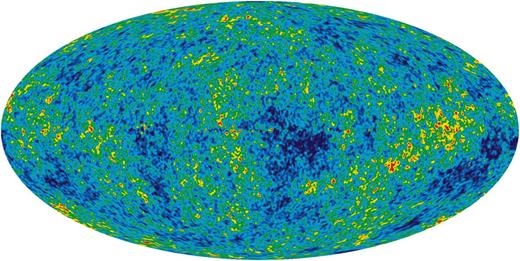
The cosmic microwave radiation map of the 13.77 billion-year-old universe. Color differences indicate temperature fluctuations within a range of ±200 microKelvin. The map enabled the proportion of matter, dark matter, and dark energy to be estimated as 5.6%, 24%, and 71.4%, respectively. The map enabled composition as well as interactions among the components of the universe to be inferred. The dark energy explains many cosmologic observations, including the flat topology. Image from the NASA/WMAP Science Team.
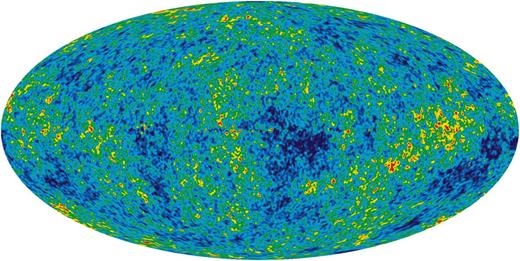
The cosmic microwave radiation map of the 13.77 billion-year-old universe. Color differences indicate temperature fluctuations within a range of ±200 microKelvin. The map enabled the proportion of matter, dark matter, and dark energy to be estimated as 5.6%, 24%, and 71.4%, respectively. The map enabled composition as well as interactions among the components of the universe to be inferred. The dark energy explains many cosmologic observations, including the flat topology. Image from the NASA/WMAP Science Team.
Acknowledgments
M.A.G. is supported by grants from the National Institutes of Health (NIH; DK092883) and the Cancer Prevention and Research Institute of Texas. L.A.G. is supported by NIH grants CA156139 and HG006367.
Authorship
Contribution: M.A.G. and L.A.G. wrote and edited the text.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Margaret A. Goodell, Department of Pediatrics, Baylor College of Medicine, Houston, TX 77030; e-mail: Goodell@bcm.edu; and Lucy A. Godley, Department of Medicine, University of Chicago, Chicago IL, 60637; email: lgodley@medicine.bsd.uchicago.edu.
