Abstract
The clinical diagnosis of acute pulmonary embolism (PE) is frequently considered in patients presenting to the emergency department or when hospitalized. Since symptoms are a-specific and the consequences of anticoagulant treatment are considerable, objective tests to either establish or refute the diagnosis have become a standard of care. Computed tomographic pulmonary angiography (CTPA), which has replaced pulmonary angiography as first-line imaging test, is associated with radiation exposure, several complications resulting from contrast dye administration, and over diagnosis. Importantly, CTPA can be avoided in 20% to 30% of patients who present with a first or recurrent episode of clinically suspected acute PE by using a standardized algorithm. This algorithm should always include a clinical decision rule to assess the likelihood that PE is present, followed by a D-dimer blood test and/or CTPA. The aim of this review is to provide clinicians this practical diagnostic management approach using evidence from the literature.
Introduction
Clinically suspected acute pulmonary embolism (PE) is frequently encountered in general practice as well as in the hospital setting. Together with acute deep-vein thrombosis (DVT), PE has been recognized as the third most common cardiovascular disorder in industrialized countries.1 The diagnostic pathway of acute PE is guided by 2 principles. First, accurate and fast identification of patients who have PE is critical because PE is a potentially fatal condition and anticoagulation is associated with the risk of major bleeding. A false diagnosis thus exposes patients to unnecessary risk of death from PE or of bleeding, which can also be fatal. Second, the use of individual diagnostic tests in isolation may lead to mismanagement of suspected PE. For these reasons, integrated diagnostic approaches that include a combination of different diagnostic tests are preferred. Here we focus on hemodynamically stable patients, who represent over 95% of all patients with symptomatic acute PE. Based on the clinical cases of 3 patients who recently presented to our hospital, we review the literature and discuss the latest evidence as well as the most current optimal treatment strategies.
Case 1
A 69-year-old male with a history of mild chronic obstructive pulmonary disease presents to the emergency department with acute-onset dyspnea. He does not report coughing, fever, or symptoms of DVT. On physical examination, he is hemodynamically stable and no abnormalities at auscultation of the heart and lungs are observed. His electrocardiogram (ECG) reveals a sinus rhythm of 60 beats/min, with a S1Q3T3 pattern. A chest radiograph is normal. The attending physician considers acute PE as a possible explanation for his symptoms. What would be the next diagnostic step?
Clinical probability assessment and d-dimer tests
The clinical presentation of acute PE varies widely among patients. While the majority of patients present with rapid-onset dyspnea or pleuritic chest pain, wheezing or a nonproductive cough are the only symptoms in some patients.2 The initial clinical evaluation includes risk factor consideration, physical examination, results from blood tests, ECG monitoring, and chest radiographs. Although nonspecific for PE diagnosis, these items are of considerable value when identifying patients in whom acute PE might be present. If acute PE is still considered after initial evaluation, further diagnostic workup should start with a standardized estimation of the likelihood of PE being present using a validated clinical decision rule. This estimation is important because, in accordance with the Bayes’ theorem, when combined with knowledge of the diagnostic test’s accuracy, it is possible to make a probability estimate that the patient has PE. Since there is no test with 100% sensitivity and/or specificity, only knowledge of the pretest probability of PE and the accuracy (sensitivity/specificity) of the available diagnostic test can be used for the most optimal (ie, safe and effective) diagnostic workup for each patient.
Two widely validated clinical decision rules for establishing the clinical probability of acute PE are available. The Wells rule consists of 7 variables (Table 1), including a judgment of whether PE is the most likely diagnosis.3 Using this rule, patients are classified as “PE unlikely” (≤4 points, 2.3%-9.4% PE risk) or “PE likely” (>4 points, 28%-52% PE risk).3 The revised Geneva score contains virtually the same items (Table 1) except for a clinical subjective judgment of the likelihood of PE.4,5 Patients with an unlikely clinical probability according to this rule (≤2 points) have a 13% to 19% PE risk; patients with a likely probability (>2 points) have a 28% to 35% PE risk.4-6 For practical purposes, both rules have been simplified by assigning only 1 point to each item (Table 1) without a resulting decrease in diagnostic accuracy.6-8
Clinical decision rules for suspected acute PE
| Item . | Original . | Simplified . |
|---|---|---|
| Revised Geneva score | ||
| Previous DVT or PE | 3 | 1 |
| Heart rate 75–94/min | 3 | 1 |
| Heart rate ≥95/min | 5 | 2 |
| Surgery or fracture <1 mo | 2 | 1 |
| Hemoptysis | 2 | 1 |
| Active malignancy | 2 | 1 |
| Unilateral lower limb pain | 3 | 1 |
| Pain on lower limb deep vein palpation and unilateral edema | 4 | 1 |
| Age >65 y | 1 | 1 |
| Clinical probability | ||
| PE unlikely | ≤5 | ≤2 |
| PE likely | >5 | >2 |
| Wells rule | ||
| Previous PE or DVT | 1.5 | 1 |
| Heart rate >100/min | 1.5 | 1 |
| Surgery or immobilization <4 wk | 1.5 | 1 |
| Hemoptysis | 1 | 1 |
| Active malignancy | 1 | 1 |
| Clinical signs of DVT | 3 | 1 |
| Alternative diagnosis less likely than PE | 3 | 1 |
| Clinical probability | ||
| PE unlikely | ≤4 | ≤1 |
| PE likely | >4 | >1 |
| Item . | Original . | Simplified . |
|---|---|---|
| Revised Geneva score | ||
| Previous DVT or PE | 3 | 1 |
| Heart rate 75–94/min | 3 | 1 |
| Heart rate ≥95/min | 5 | 2 |
| Surgery or fracture <1 mo | 2 | 1 |
| Hemoptysis | 2 | 1 |
| Active malignancy | 2 | 1 |
| Unilateral lower limb pain | 3 | 1 |
| Pain on lower limb deep vein palpation and unilateral edema | 4 | 1 |
| Age >65 y | 1 | 1 |
| Clinical probability | ||
| PE unlikely | ≤5 | ≤2 |
| PE likely | >5 | >2 |
| Wells rule | ||
| Previous PE or DVT | 1.5 | 1 |
| Heart rate >100/min | 1.5 | 1 |
| Surgery or immobilization <4 wk | 1.5 | 1 |
| Hemoptysis | 1 | 1 |
| Active malignancy | 1 | 1 |
| Clinical signs of DVT | 3 | 1 |
| Alternative diagnosis less likely than PE | 3 | 1 |
| Clinical probability | ||
| PE unlikely | ≤4 | ≤1 |
| PE likely | >4 | >1 |
In patients with an unlikely probability, a d-dimer test can be applied to rule out PE. Fibrin d-dimer is a marker of fibrinolysis, and d-dimer levels are typically elevated in patients with acute thrombotic disease. Other clinical conditions associated with enhanced fibrin formation, such as malignancy, trauma, disseminated intravascular coagulation, infection, and postoperative states, also can give rise to elevated d-dimer levels. Hence, the sensitivity of a dimer test for acute PE is very high yet it has poor specificity.9 In general, the d-dimer threshold for a normal test result is 500 µg/L, although 3 recent post-hoc analyses have suggested that an age-dependent cutoff, defined as patient age × 10 μg/L (only for patients age >50 years), is safe and more efficient for use in clinical practice.10-12 A prospective management study to confirm the safety of this age-dependent cutoff is currently under way. Its results are expected by the end of 2013.
The combination of a normal, high-sensitivity, quantitative d-dimer test result and an unlikely clinical probability has enough negative predictive value to rule out acute PE without further imaging. For the original Wells rule, a meta-analysis that includes all high-quality prospective management studies confirmed the very low 3-month venous thromboembolism (VTE) risk in 1660 consecutive patients with an unlikely probability and a normal d-dimer. The pooled negative predictive value was 99.7% (95% confidence interval [CI], 99.0-99.9).13 The PE-related 3-month mortality risk in these patients was very low as well (0.06%; 95% CI, 0.0017-0.46).13
In the recent Prometheus study, both the original and the simplified Wells rule and revised Geneva score were, for the first time, directly compared in 807 consecutive patients.6 The 4 decision rules showed similar performance for exclusion of acute PE in combination with d-dimer testing. The 3-month VTE recurrence rates of all 4 scores ranged from 0.5% to 0.6%. Since none of the 4 rules has been proven to be superior, the choice for a specific rule is dependent on local preference. Notably, a d-dimer test lacks the sensitivity to safely rule out PE in patients with a likely probability. Therefore, all patients with an elevated d-dimer or a clinical decision rule indicating “likely probability” should be referred for radiological evaluation. Finally, the indiscriminate use of clinical probability scores or d-dimer assays as a screening test for PE in the workup of unselected patients with respiratory or chest symptoms will lead to a large number of false-positive test results and therefore result in excessive and unneeded diagnostic testing.
Computed tomography pulmonary angiography
Computed tomography pulmonary angiography (CTPA) has become the first-line imaging method for assessment of patients with clinically suspected acute PE. CTPA is readily available in most hospitals and has been shown to have high sensitivity and specificity for PE, comparable with the traditional gold standard of invasive pulmonary angiography. The sensitivity is dependent on thrombus location and clot burden as well as on the number of CT detector rows. Sensitivity ranges from 20% to 30% for small, distal, subsegmental emboli using single-row CTPA to >95% for segmental, lobar, and centrally located pulmonary emboli using multirow-detector (MD) CTPA.14-17 Numerous management studies have shown that CTPA can be used as a single diagnostic test to rule out or establish acute PE. A meta-analysis of 23 studies with a total of 4657 patients found a 3-month VTE event rate after negative CTPA of 1.4% (95% CI, 1.1%-1.8%) and a 3-month fatal PE rate of 0.51% (95% CI, 0.33%-0.76%).18 The safety of CTPA as a single imaging test has been further established by a randomized noninferiority trial in which compression ultrasonography of leg veins in addition to MD-CTPA did not lead to better results in excluding PE.19
This evidence has strongly supported the widespread implementation of CTPA. However, several concerns can be raised regarding the lowered threshold and increased frequency of CTPA use. First, overuse of CTPA as the first and only diagnostic test in patients suspected of PE leads to a very low prevalence (<10%) of diagnosed PE.20 This low diagnostic yield seems consistent with a trend of overdiagnosis because of an observed rise in PE incidence with minimal change in mortality and lower case fatality since the introduction of CTPA.21 Second, there is increasing fear of long-term radiation complications, allergic reactions to iodinated contrast material, and contrast-induced nephropathy.15,22,23 Finally, smaller subsegmental emboli are more frequently detected. Although observational research suggests that treated patients with subsegmental PE as well as untreated patients with subsegmental PE have a good prognosis, the true clinical relevance of these emboli remains uncertain.24-26
Taken together, it is imperative that the use of CTPA is limited to those patients with a clear indication for CTPA, that is, patients with a high clinical probability or an elevated d-dimer level in whom PE cannot be ruled out without performing radiological imaging. The diagnostic safety for excluding PE in these selected patients has been confirmed in several outcome studies where only patients with either an elevated d-dimer level or a likely clinical probability were subjected to CTPA,19,27,28 with a pooled 1.2% (95% CI, 0.8%-1.8%) risk for recurrent VTE during the 3 months following a negative CTPA.29 The risk for fatal PE was consistently low (0.6%; 95% CI, 0.4%-1.1%).29
Integrated approach
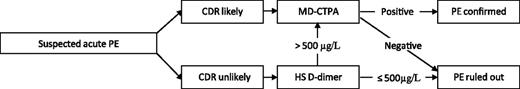
In most cases, an integrated diagnostic algorithm is used for the diagnostic workup of suspected PE in order to reduce the number of unnecessary radiological imaging tests as well as to keep the 3-month VTE failure rate below 2%. These are the rates of VTE detected during follow-up after use of invasive pulmonary angiography or CTPA. We recommend a strategy that starts with clinical probability assessment by means of a validated clinical decision rule. In case of unlikely clinical probability, a d-dimer test should be ordered. Only with a normal test result can PE be ruled out and the patient be safely left untreated. If the decision rule indicates “PE likely” or if d-dimer levels are elevated above the threshold, the patient should be referred for CT scanning and be further managed according to the CTPA result. Using this algorithm (Figure 1), CTPA can be avoided in 20% to 30% of patients with suspected acute PE, and an effective management decision can be made for 98% of patients.27,30
Preferred diagnostic algorithm for clinically suspected acute PE. CDR, clinical decision rule; HS, highly sensitive.
Preferred diagnostic algorithm for clinically suspected acute PE. CDR, clinical decision rule; HS, highly sensitive.
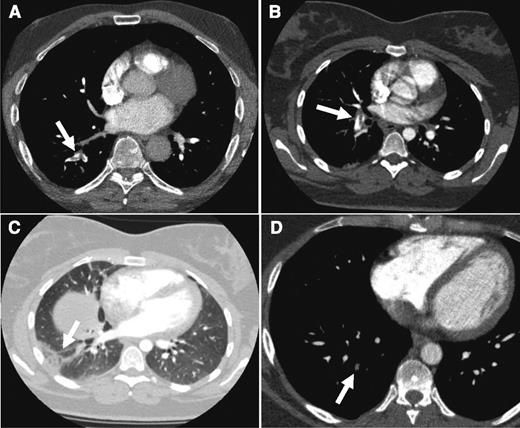
As for our patient, both the Wells rule and the revised Geneva score indicated an unlikely probability (Wells score: 3 points for PE as the most likely diagnosis; revised Geneva score: 1 point for age >65 years). Subsequent laboratory testing revealed an elevated d-dimer level of 2200 µg/L. Even when an age-dependent cutoff was applied (age 69, adjusted d-dimer cutoff 69 × 10 = 690 µg/L), this concentration was well above the normal threshold. Consequently, the patient was subjected to CTPA that confirmed a fresh embolus in the segmental artery to the right lower lobe (Figure 2A).
CTPA results from the cases. CTPA of patients from case 1 (A: arrow indicates acute thrombus in segmental artery to the right lower lobe), case 2 (B: despite breathing artifacts, clear visualization of acute PE in right segmental artery; C: arrow shows a wedge-shaped peripheral consolidation indicative of pulmonary infarction), and case 3 (D: arrow points to an organizing mural thrombus in a right basal segmental pulmonary artery).
CTPA results from the cases. CTPA of patients from case 1 (A: arrow indicates acute thrombus in segmental artery to the right lower lobe), case 2 (B: despite breathing artifacts, clear visualization of acute PE in right segmental artery; C: arrow shows a wedge-shaped peripheral consolidation indicative of pulmonary infarction), and case 3 (D: arrow points to an organizing mural thrombus in a right basal segmental pulmonary artery).
Case 2
A 22-year-old previously healthy, although obese, woman is admitted to the emergency ward with acute-onset right-sided chest pain. She remembers coughing up a small amount of blood earlier that morning but denies a fever or mucus production. She was recently prescribed an oral contraceptive because of menorrhagia. On examination, the attending clinician notices a tachycardia of 130 beats/min. The chest radiograph is of poor quality because of her obesity and because the chest pain prohibited her from holding her breathe. The radiograph shows signs of a subtle right-side paracardial consolidation. Because acute PE is high in the differential diagnosis, the Wells score is calculated (5.5 points; revised Geneva score 7 points), and it is concluded that she can be categorized as PE likely. Because there is concern of radiation exposure in this young woman, the physician questions whether there are alternative radiological options other than CTPA.
Ventilation-perfusion scintigraphy
In the past 3 decades, the total number of CT scans performed for any indication has grown exponentially. In fact, more than 70 million CT scans were performed in the United States in 2007.31 It has been postulated that CT scan–associated radiation may increase an individual’s lifetime risk of developing cancer. The organs in the field of view (breasts, esophagus, heart, and lungs) are exposed to the overall highest absorbed doses and hence are at highest risk. The radiation dose of a single CTPA ranges from 3 to 5 mSv, with an estimated risk of 150 excess cancer deaths per million exposures to a single CTPA.15,32,33 The risk of CT-associated cancer is especially of interest for the young female patient because the lifetime attributable risk, especially for breast cancer, rises exponentially with exposure at younger age.31-33
Concerning acute PE, an alternative to CTPA is ventilation-perfusion (V-Q) lung scintigraphy, which involves the simultaneous scintigraphic imaging of the pulmonary arteries and airways, with exposure to a radiation dose of 1.2 mSv.34,35 A normal V-Q scintigram, one with no perfusion defects, virtually rules out PE with a 3-month failure rate of 0.9% (upper 95% CI, 2.3%).35,36 A V-Q scintigram showing at least 1 segmental perfusion defect combined with a normal ventilation scan, the so-called high-probability lung scan, has a 85% to 90% predictive value for PE.35,36 The main drawback of V-Q scintigraphy is the large proportion of nondiagnostic scan results when both perfusion and ventilation defects are present in the same anatomic area, being reported to occur in 28% to 46% patients.37 Since the PE prevalence in that specific cohort is 10% to 30%, further imaging with CTPA is warranted. Several potential solutions have been proposed to deal with this issue. For instance, by applying adjusted ruling criteria, the so-called PISAPED criteria (Prospective Investigative Study of Acute Pulmonary Embolism Diagnosis), the number of nondiagnostic V-Q scintigraphy results is likely to decrease.38 Limiting the number of nondiagnostic lung scans can also be achieved by performing V-Q scintigraphy only in patients with normal chest radiographs. Moreover, the sensitivity and specificity of the combination of perfusion scintigraphy and chest radiograph, the so-called X-Q combination, without adding ventilation lung scanning, was found to be 80% to 85% and 93% to 97%, respectively.38,39 Notably, only post-hoc analyses regarding both the PISAPED criteria and the X-Q combination are available, and formal outcome studies are lacking. The same is applicable for 3-dimensional images acquired by single-photon emission computed tomography (SPECT), a technique that may improve V-Q scintigraphy by applying a γ-emitting radioisotope.40
Magnetic resonance pulmonary angiography
Magnetic resonance pulmonary angiography (MRPA) is a potentially attractive method for PE imaging because ionizing radiation is not used. In addition, nephrotoxicity and contrast allergies caused by gadolinium-based contrast agents are less of a concern, especially in young patients with normal renal function. In preliminary studies with limited sample sizes, sensitivities of 77% to 100% and specificities of 95% to 98% were observed when compared with conventional pulmonary angiography.41,42 More recently, 2 large cohort studies were performed in which MRPA was directly compared with CTPA and with V-Q scintigraphy.43,44 Both studies confirmed the high diagnostic accuracy of MRPA for acute PE, although a limitation of MRPA was noted, that is, a disturbing 25% to 30% of scans were nondiagnostic.43,44 MRPA requires prolonged breath-holding, which is difficult for patients in respiratory distress. Breathing, or motion artifacts, and poor arterial opacification of segmental and subsegmental branches are the most prevalent reasons for a noninterpretable MRPA.45 Moreover, MRI may not be tolerated by patients with claustrophobia and is contraindicated during pregnancy and when intracranial vascular clips, metal implants, or cardiac pacemakers are present. Taking these contraindications together, the majority of potentially eligible patients had to be excluded from the 2 studies.43,44 Finally, since there are no reports of patients being managed based on MRPA result alone, MRPA cannot be recommended as an alternative to CTPA in the diagnostic workup of suspected PE yet.
In conclusion, CTPA is associated with an actual health risk, although the absolute risk of cancer is probably small. Nevertheless, V-Q scintigraphy as well as MRPA are associated with a considerable chance for a nondiagnostic test, resulting in the need for repeated radiological examinations with associated costs, further radiation exposure, and other complications. The safety of promising alternative techniques, including MRPA, X-Q scanning, and SPECT, has yet to be confirmed in management studies. From an individual standpoint, if a CT scan is justified by a strong medical indication, the associated cancer risk is small relative to the value of the diagnostic information that can be obtained. From a population standpoint, use of CT examinations and the resultant cancer risk could be reduced by adhering to appropriate-use criteria.
With this in mind, the patient was informed of the suspected PE and the potential risks of radiation exposure. She agreed to CTPA, which showed a large embolus in a right segmental pulmonary artery (Figure 2B). A wedge-shaped, pleural-based opacity in the right lower lobe indicated the concomitant presence of pulmonary infarction (Figure 2C).
Case 3
The third patient is a 52-year-old man with a prior history of an unprovoked acute bilateral PE 4 years ago. He noticed a progressive sharp pain on the left side of his back with every deep breath. Initially, he thought that he had torn a muscle while painting his garden house. Since his symptoms persisted for 2 days and he recognized this particular pain from his first thromboembolic episode, he decided to visit his general practitioner who referred him to our outpatient clinic to rule out recurrent PE. Physical examination revealed no abnormalities. Chest radiograph and ECG were normal as well. His pain could be provoked by firm pressure on the seventh and eighth left ribs. Consequently, a musculoskeletal cause of the pain was judged most likely, although recurrent PE could not be ruled out. Both the Wells rule (1.5 points for previous PE) as well as the revised Geneva score (3 points for previous PE) indicated PE unlikely. Because the subsequently assessed d-dimer level was 910 µg/L, the patient was referred for CTPA, which showed 1 small organizing mural thrombus in a right basal segmental pulmonary artery. No intrapulmonary or ossal irregularities were observed. Since his first acute PE was confirmed in a different hospital, we had no earlier CTPA results for comparison. Nonetheless, the radiologist’s final conclusion was “no signs of an acute pulmonary thrombus, only evidence of residual emboli.” At this point, can we safely discharge this patient without anticoagulant treatment?
Recurrent PE
Most large trials on the diagnostic management of acute PE have not included patients with suspected recurrent PE. Diagnosing recurrent PE can be challenging for several reasons. First, it has been suggested that both sensitivity and specificity of d-dimer assays for recurrent PE are decreased.46 Second, recurrent emboli may be difficult to differentiate from residual chronic emboli, which may persist in 20% to 40% of patients after an initial PE episode.47,48 In 2 post-hoc analyses, the safety of ruling out recurrent PE based on an unlikely clinical probability and a normal d-dimer test was evaluated. Both studies had a 0% failure rate during 3-month follow-up but with very high upper 95% CI (6.9% and 7.9%, respectively) due to a relatively small sample size.46,49 A recent prospective trial included 516 consecutive patients with suspected recurrent PE.50 Of these, 182 were classified PE unlikely. Based on a normal d-dimer result, 88 were left untreated. None of the 88 patients were diagnosed with recurrent DVT or PE in the subsequent 3 months (0%; 95% CI, 0.0%-3.4%). On the other hand, recurrent VTE was diagnosed during 3 months of follow-up in 3.2% (95% CI, 1.5%-5.9%) of the patients with a negative CTPA result, which is more than twice as high as the 1.2% (95% CI,, 0.8%-1.8%) in a population with primarily initial PE.29 Whether this discrepancy can be explained by failure of the CTPA or an intrinsic higher thrombotic risk is a matter of debate. In case of a normal CTPA but a high clinical suspicion of recurrent PE, either ultrasonography of the legs or conventional angiography can be considered, although there is no evidence available to validate such a strategy. Perhaps the most pragmatic approach would be to closely monitor these patients in an inpatient or outpatient setting, dependent on their condition.
The latter strategy was applied to our patient. Based on the discrepancy between the location of the pain and the location of the chronic embolus, we judged the presence of acute recurrent PE to be very unlikely, instructed him in which circumstances he had to contact the hospital, and prescribed a nonsteroidal anti-inflammatory drug (NSAID) to ease the pain, which we considered to be of musculoskeletal origin. We advised his general practitioner to monitor him in the following days and arranged a follow-up visit at our outpatient clinical 2 weeks later. At that time, the pain had completely resolved and he had stopped taking the NSAID. Six months after initial presentation, the patient was doing well and did not report any new symptoms of recurrent DVT or PE in the intervening period.
Conclusion
A diagnostic strategy that starts with the assessment of clinical probability and is followed by either d-dimer testing or CTPA is a safe and effective management strategy for patients with a suspected first or recurrent acute PE. Strict adherence to this algorithm, which has been validated in many high-quality trials evaluating well over 5000 consecutive patients, will limit the number of unnecessary imaging tests by 20% to 30%, with an associated reduction in health care costs and complications.
Authorship
Contribution: M.V.H. and F.A.K. wrote and reviewed the manuscript and reviewed and approved each other’s sections.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: M. V. Huisman, Leiden University Medical Center (C-7-Q), Albinusdreef 2, 2300 RC, Leiden, The Netherlands; email: m.v.huisman@lumc.nl.