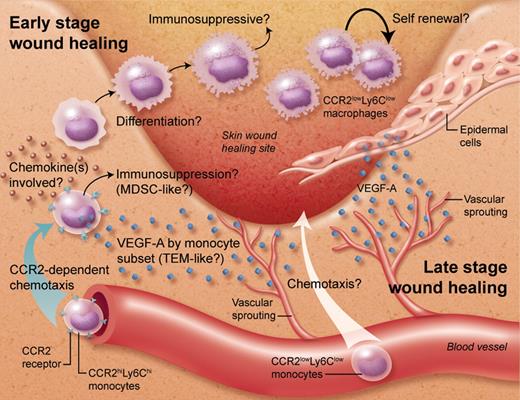
In this issue of Blood, Willenborg and colleagues uncover the timeline of monocyte/macrophage involvement during sequential phases of skin wound healing.1 The CCR2-mediated recruitment of a vascular endothelial growth factor A (VEGF-A)–expressing inflammatory monocyte subset is critical for early vascular sprouting, while epidermal-derived VEGF-A mediates vascularization in the late wound healing phases (see figure).
The involvement of CCR2-mediated monocyte recruitment and monocyte-derived VEGF-A in early vessel sprouting during skin wound healing. At later stages, more mature macrophages are found and VEGF-A production switches to epidermal cells. Professional illustration by Alice Y. Chen.
The involvement of CCR2-mediated monocyte recruitment and monocyte-derived VEGF-A in early vessel sprouting during skin wound healing. At later stages, more mature macrophages are found and VEGF-A production switches to epidermal cells. Professional illustration by Alice Y. Chen.
Macrophages are monocyte-derived phagocytes that are the jacks-of-all-trades in our body. These cells display a remarkable functional polyvalency and ability to adapt to changes in the microenvironment, due to their vast receptor repertoire that continuously senses the surroundings, and their versatile biosynthetic capacity. Consequently, these cells play central roles in seemingly opposite physiologic processes. For example, macrophages are responsible for the recognition, uptake, and destruction of micro-organisms leading to the initiation of inflammation (immunologic role of macrophages), while also being crucial for tissue restoration during wound healing that conversely requires a dampening of overt inflammation (trophic role of macrophages), as further evidenced in the report by Willenborg et al.1
Further adding to the complexity and heterogeneity of the mononuclear phagocyte system is the existence of distinct monocyte subsets that differ in molecular repertoire, in vivo behavior, and possibly also differentiation potential. The chemokine receptor CCR2 has not only been proven useful as a discriminative marker between inflammatory/classical monocytes (CCR2+Ly6Chigh) and resident/patrolling/nonclassical monocytes (CCR2−Ly6Clow),2 but it is also actively participating in the recruitment of the former subset to sites of infection, trauma, or tumor formation. However, interpretation of data using CCR2-deficient mice is never trivial, because this receptor is necessary for CCR2+Ly6Chigh monocyte emigration from the bone marrow and its absence provokes monocytopenia in the blood.3 Willenborg et al elegantly solve this issue using a novel cre/lox-based mouse strain that allows the ablation of CCR2 functionality under the control of the Lysozyme M (LysM) promoter. This promoter is less active in bone marrow monocytes, allowing their normal exit to the circulation, where LysM activity increases and CCR2 deficiency becomes more complete.1
With this tool, the authors unequivocally demonstrated the importance of CCR2 for attracting peripheral blood Ly6Chigh monocytes to the site of excision wound injury, where they play a nonredundant role in early-phase angiogenesis via the production of VEGF-A. This finding raises a number of questions. CCR2 is the receptor for several chemokines—CCL2, CCL7, CCL8, CCL12, CCL16—and it remains to be seen which of these ligands is the main monocyte attractant, and which cells start producing the(se) ligand(s) in response to injury. In addition, despite being of key importance, the VEGF-A production is limited to a minority of the infiltrating Ly6Chigh monocytes, suggesting functional specialization. An interesting issue in this respect is whether pre-existing VEGF-A–expressing monocytes are attracted to the wound, or whether a subset of monocytes are “edited” in situ to perform this function. This is reminiscent of the situation in tumor biology (as a matter of fact, tumors have been described as “wounds that never heal,” highlighting the mechanistic parallels between wound healing and tumor progression4 ), where tumor-infiltrating monocytes and macrophages have been shown to control the angiogenic switch, but distinct macrophage subsets might differentially contribute to this phenomenon.5 In particular, Tie2-expressing monocytes (TEMs) are a subset of angiogenesis-committed myeloid cells in the blood and in tumors,6 and it seems, therefore, tempting to speculate that the VEGF-A–producing wound monocytes share many similarities with TEMs. Finally, it needs to be determined whether the current findings translate to other types of (skin) damage, as model-specific differences for the implication of myeloid-derived VEGF-A have been reported.7
Interestingly, angiogenesis and immune suppression often go hand-in-hand, sharing similar molecular and cellular mediators.8 Also in the context of wound healing, immune-suppressive cells would come in handy as safeguards against inappropriate immune reactivity toward endogenous danger signals. Cells such as myeloid-derived suppressor cells (MDSCs), which include a monocytic (MO)–MDSC and a granulocytic polymorphonuclear (PMN)–MDSC fraction,9 are best known for their ability to suppress the activation of various lymphoid and myeloid cell types, but are also potently pro-angiogenic. Although the authors argue that the early wound-infiltrating monocytes do not fully comply with MO-MDSC surface marker expression, the ultimate test would be to assess their T-cell suppressive capacity.
Later stages of the wound healing process are characterized by a dominance of large, granular CCR2lowLy6Clow myeloid cells, which is more consistent with the phenotype of mature macrophages. It is tempting to speculate that these macrophages are the progeny of the initial CCR2+Ly6Chigh monocyte infiltrate, similar to what has been observed in growing tumors.5 However, one cannot formally exclude the contribution of distinct monocyte subsets to the sequential skin wound healing phases, a mechanism that seems to be required for a normal healing of the injured myocardium.10 In addition, it would be interesting to investigate whether this pool of later stage wound macrophages is the mere result of monocyte infiltration and differentiation, or whether local proliferation of these tissue macrophages11 contributes as well. A remarkable observation is the switch in the VEGF-A origin from myeloid to epidermal in the course of wound healing. This illustrates the importance of correctly timed and probably also correctly localized VEGF-A production during tissue regeneration. As a matter of fact, the inappropriate production of VEGF-A by macrophages might lead to immature and dysfunctional vessels,12 which would hamper the healing process.
The strictly timed interplay of cells and molecules in the course of wound healing as demonstrated in the report by Willenborg et al might not facilitate therapeutic intervention, for example, to correct healing deficiencies. The risk exists that any therapy (at the level of monocyte or VEGF availability, for example) might be given too early, too late, too much, or too little, and hence not yielding the desired effects. However, this report is setting the stage for further exploring the wound healing process and the identification of additional players involved.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal