Abstract
Abstract  962
962
Most patients with relapsing-remitting multiple sclerosis (RRMS) do not achieve a sustained remission after disease-modifying therapy. A phase II clinical trial of high-dose immunochemotherapy (HDIT; BCNU, etoposide, ara-C, melphalan and antithymocyte globulin) and autologous hematopoietic cell transplantation (HCT) was conducted in patients with highly active RRMS who had failed conventional therapy to assess if a high rate of sustained remission could be induced. Eligibility required an EDSS of 3.0 (moderate disability, fully ambulatory) to 5.5(severe disability, ambulatory only 100 meters without aids) and >2 relapses on treatment in previous 18 months. Treatment-failure was defined as a composite endpoint including 1) mortality 2) relapse 3) new MRI lesions or 4) disability increase >0.5 EDSS points. Adverse events (AE) were recorded according to NCI-CTCAE v3.0.
25 patients at a median age of 38(27-53) years were treated with G-CSF to mobilize the autograft; prednisone was given at the same time to prevent MS flares. The autograft was CD34-selected (Baxter, Isolex). One patient withdrew after mobilization secondary to HIT/pulmonary embolus. 24 patients had HDIT/HCT according to protocol. Median follow-up was 131 (52, 282) weeks. After initially stabilizing, one patient died from progressive loss of neurological function at 32 months. No patient had delayed recovery of blood counts. In the 1st year after HDIT, there were 42 grade 3 and 6 grade 4 non-hematopoietic AE. Grade 4 AE included: one suicide attempt (with 3 grade 4 AE); hyperuricemia; hypokalemia; and elevated ALT. In the 2ndyear, there were 13 grade 3 and 1 grade 4 non-hematopoietic AE. The 1-year and 2-year probabilities of event-free survival (i.e. without treatment-failure) were 95.8% (90% CI: 80.2%-99.2%) and 82.8% (90% CI: 65.0%-92.0%), respectively. Progression-free and relapse-free survival at 1 year were 100% (90% CI: 100%-100%) and 95.8% (90% CI: 80.2%-99.2%) and at 2 years were 91.7% (90% CI: 75.7%-97.3%) and 91.7% (90% CI: 75.7%-97.3%), respectively. The probability of freedom from disease activity detected by brain MRI was 95.8% (90% CI: 80.2%-99.2%) at both year 1 and 2. In comparison, a randomized clinical trial of placebo vs natalizumab (Havrdova E et al, Lancet Neurology, 2009) showed that 7% and 37% of RRMS patients were free of disease activity (i.e. progression, relapse and MRI) at 2 years, respectively.
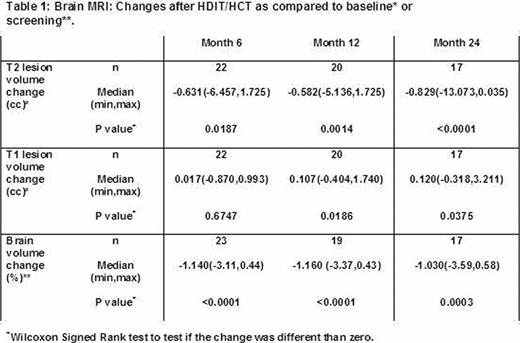
T2-weighted MRI scans measure disease burden from MS. T2 lesion volume was significantly reduced by 6 months and was sustained at 2 years (Table 1). T1 lesion volume was increased at 1 year. There was a significant loss of brain volume at 6 months but stabilized after this time point.
Flow cytometry of peripheral blood was done at baseline and at 1, 2, 6 and 12 months. There was near complete depletion of naïve CD4 and CD8 T cells (CD45RA+) at 1 month. Memory CD4 and CD8 T cells (CD45RO+) were not completely eliminated from the blood after in vivo depletion from HDIT. Within 2 months of transplant, there was rapid expansion of memory CD8 T cells. The numbers of CD4 naïve and memory T cells were not recovered at 1 year. CD4 and CD8 recent thymic emigrants (CD45RA+, CD31+) were increased at 1 year compared to the nadir at 1 month but did not completely recover. Recovery of naïve and memory B cells was complete between months 6 and 12.
HDIT/HCT for highly active RRMS resulted in profound immunosuppression and induced a high rate of sustained remissions at 2 years. The small increase in T1-weighted lesion volume in the absence of persistent brain inflammation may have resulted from damage due to previous brain injury. No further loss in brain volume was observed after 6 months. Follow-up is planned through 5 years.
Brain MRI: Changes after HDIT/HCT as compared to baseline* or screening**.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal