Abstract
Abstract 958
Primary graft failure (pGF) is associated with considerable morbidity and mortality in hematopoietic stem cell transplantation (HSCT). Salvage HSCT can rescue pGF patients, however, prospective controlled trials are difficult and the optimal preconditioning regimen and stem cell source have not been established, because of the rarity of pGF and emergent condition of the patients.
In this study, to investigate prognostic factors of salvage allogeneic HSCT and to obtain fundamental information for establishing a standard approach for pediatric pGF, we performed retrospective analysis of a salvage HSCT for pGF after allogeneic HSCT in children. A total of 102 patients were analyzed based on data reported to the Japan Society for Hematopoietic Cell Transplantation (JSHCT) registry. The patients were selected according to the following criteria: (1) aged 18 years or younger at salvage HSCT; (2) engraftment not achieved by a prior allogeneic HSCT, and salvage allogeneic HSCT performed; (3) salvage HSCT performed within 60 days after the first HSCT; (4) both the first and salvage HSCTs performed between 1982 and 2010.
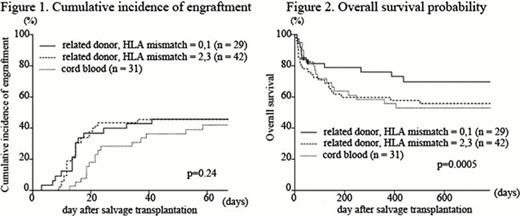
The median follow-up period in the surviving patients was 1502 days (range, 37–9101) after salvage HSCT. The estimated OS probability and standard error at 1 year after salvage HSCT was 53.3% ± 5.0%. The cumulative incidence of engraftment at 60 days was 55.7% ± 5.0%, whereas non-relapse mortality (NRM) at 1 year was 31.7% ± 4.7.
Donor sources of the 102 salvage HSCT were 29 of HLA matched or 1-antigen mismatched related donor (rMM01), 42 of HLA 2- or 3-antigen mismatched related donor (rMM23), and 31 of cord blood (CB). The engraftment rate at 60 days was 57.7% ± 10.1% for rMM01, 57.1% ± 7.7% for rMM23, and 42.2% ± 9.4% for CBT (p = 0.24, Figure 1). The rMM01 group showed the highest OS (68.8% ± 8.6%), whereas OS was similar in the rMM23 (47.6% ± 7.7%) and CB (45.7% ± 8.6%) groups (Figure 2). The median time for neutrophil engraftment after CBT was 22 days, which was significantly longer than those for rMM01 (15 days) and rMM23 (15 days) (p = 0.02 and 0.0007, respectively).
Thirty-one salvage CBTs were performed in our cohort. The median total nuclear cell (TNC) count was 5.3 (range, 2.2–13.3) × 107 cells/kg, and the median CD34-positive cell count was 1.6 (range, 0.13–5.3) × 105 cells/kg. There was no association between the cell counts and engraftment. HLA antigen mismatch did not result in inferior engraftment.
Fludarabine, alkylating agents, anti-thymocyte/lymphocyte globulin, and irradiation were frequently used with various combinations, and all these components provided better engraftment probability. Alkylating agents was associated with better survival rate (p = 0.004).
Multivariate analysis showed that rMM01 was significantly correlated with better engraftment and survival. The hazards for engraftment and survival were not different between rMM23 and CBT. Multivariate analysis showed also an advantage of FLU and irradiation in engraftment. On the other hand, alkylating agents had a major impact on survival probability, and the usage of alkylating agents was related with superiority in survival.
A previous report including a small number of pediatric pGF patients showed an advantage of PBSC from mismatched related donors, whereas our analysis demonstrated that the survival curve for CBT was superimposed on the curve for HSCT from a mismatched related donor, although engraftment achievement tended to be lower and engraftment was later. In our cohort, the median TNC count of CB was considerably higher than that reported previously. The small body size of children allows a relatively high number of CB to be obtained.
Of note, this study was a retrospective and uncontrolled study. Further prospective studies in a large cohort are therefore required to further improve the treatment of pediatric pGF patients.
In conclusion, our study provides valuable information on the role of the second salvage HSCT for pediatric pGF. This study included the largest number of children with pGF investigated till date, and showed that rMM01 donor was the most suitable donor for salvage HSCT, and that CBT was an equally important option compared with a haploidentical related donor for patients without a well matched related donor.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal