Abstract
Abstract 817
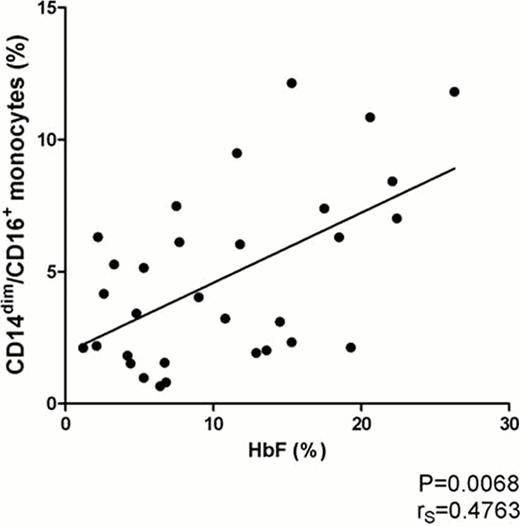
Vaso-occlusion in sickle cell anemia (SCA) involves inflammation and cell activation; fetal hemoglobin (HbF) elevation by hydroxyurea (HU) remains the mainstay of SCA treatment. Monocytes are activated in SCA, and their contribution to the chronic inflammatory state includes the production of cytokines and reactive oxygen species (ROS). Monocytes are a heterogeneous group of leukocytes subdivided into distinct subsets: classical monocytes comprise over 80% of circulating monocytes, are highly positive for CD14 (CD14bright) and typically CD16-negative, while CD16-positive monocytes have been further subdivided into intermediate CD14bright/CD16+, and non-classical CD14dim/CD16+ monocytes. Intermediate monocytes are recognized as the main monocytic producers of ROS and are increased in inflammatory conditions such as atherosclerosis and sepsis. The less characterized non-classical subset is believed to have a patrolling behavior in blood vessels, does not produce ROS and constitutively produces IL-1 receptor antagonist (IL1-RA). Another relevant subgroup of monocytes expresses angiopoietin-2 receptor TIE2, and the role of TIE2-expressing monocytes (TEMs) has been investigated in angiogenesis in neoplastic diseases. TEMs usually correspond to intermediate monocytes, but their importance in inflammation is still unclear. We hypothesized that monocyte subsets in SCA patients would differ from controls, and that treatment with HU might also influence monocyte phenotypes, thus shedding light on the possible role of these subsets in an inflammatory condition not previously studied. EDTA-anticoagulated peripheral blood samples were collected upon written informed consent from 21 healthy controls (CON, ages 21–63 years) and 34 SCA patients (18 on HU, ages 16–58 years) in steady state, with no transfusion or acute sickling episode in the previous three months. Monocytes were immunophenotyped by flow cytometry on a multicolor FACSCalibur cytometer. Medical history of SCA-associated complications, HbF levels and dosage of HU in mg/kg/day were obtained from medical charts. Statistical analysis was performed on GraphPad Prism 5.0 software. As expected, we found that relative percentage and absolute count of CD16-positive monocytes were higher in SCA patients than in controls. Surprisingly, a significantly higher percentage of non-classical CD14dim/CD16+ monocytes, rather than intermediate cells, was found in SCA patients on HU (SCA-HU) treatment (mean±SEM: CON 2.06±0.43%, SCA 2.91±0.50%, SCA-HU 6.42±0.80%, P<0.0001). TEMs were also increased in SCA patients compared to controls (CON 2.64±0.72%, SCA 20.48±5.40%, SCA-HU 32.97±5.92%, P<0.0001), but HU treatment did not significantly influence TEM counts. Mean TIE2 expression did not vary among the groups, and there was no correlation between TEMs and presence of SCA complications pathophysiologically associated with disturbed angiogenesis, such as pulmonary hypertension, osteonecrosis, leg ulcers and retinopathy. Higher percentages of non-classical monocytes in HU-treated patients were initially interpreted as a possible toxic effect of HU on monocytopoiesis, but the lack of correlation of monocytes subsets with the degree of relative monocytopenia made this hypothesis unlikely. Moreover, we found a significant positive correlation between percentages of non-classical monocytes and HbF levels (rS=0.4763, P=0.0068, see figure). This suggests that successful HU treatment with higher HbF could correlate with the expansion of this particular monocyte subset. During the study period, only one patient was available for comparison before and after HU, but the increase in HbF from 4.2% to 11.6% and in non-classical monocytes from 1.82% to 9.48%, in this case, corroborates that HU therapy may explain this phenotype shift in monocytes. Whether non-classical monocytes expansion represents yet another pleiotropic effect of HU, if these cells are less likely to take part in the vaso-occlusive process and have an antiinflammatory role or, furthermore, if a bone marrow counterpart of this monocyte subset could be involved in increasing HbF production, remains to be investigated. The correlation of the expansion of non-classical monocytes with HbF levels could prove to be an interesting biomarker of response to HU, and future studies may address its clinical usefulness.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal