Abstract
Abstract  659
659
NPM1 mutations and WT1 expression are frequently identified in acute myeloid leukemia (AML). Both markers have been reported as suitable molecular target for minimal residual disease (MRD) monitoring. Recently, Gemtuzumab Ozogamicin (GO) has been shown to improve event free survival and overall survival in adult AML.
To follow MRD in AML patients with NPM1 mutations (NPM1mut) and/or WT1 expression (WT1+) and treated in the randomized ALFA 0701 GO trial conducted by the Acute Leukemia French Association (Castaigne et al, Lancet 2012), in order to validate their prognostic significance and to evaluate the effect of GO on MRD response.
The ALFA 0701 trial included 278 patients aged 50–70 years with newly-diagnosed de novo AML, randomized to receive or not five doses of 3 mg/m2 GO, on day 1, 4 and 7 of standard induction chemotherapy and on day 1 of two consolidation chemotherapy courses, respectively. A total of 77 NPM1mut (35 in control arm, 42 in GO arm) and 178 WT1+ (87 in control arm, 91 in GO arm) AML patients were studied. WT1 + at diagnosis was defined as a ratio WT1/ABL transcript above 25% in bone marrow (BM) or 5% in peripheral blood (PB) samples. PB and BM samples were collected at diagnosis, after induction and after each consolidation course. MRD levels were assessed using cDNA-based real-time quantitative PCR (RQ-PCR) and reported as the ratio NPM1mut or WT1 transcript/100 ABL transcript. Occurrence of a MRD level below the threshold (NPM1mut <0.1% and WT1 transcript < 0.5% in PB) was defined here as a good MRD response. The prognostic value of MRD was assessed by comparing the outcome of good versus poor MRD responders after induction in terms of cumulative incidence of relapse (CIR) at 18 months. Effect of GO was then evaluated by comparing MRD response in both treatment arms.
178 patients (favorable cytogenetics: 4%, intermediate: 69%, unfavorable: 27%) were WT1+. WT1 transcript levels at diagnosis had no prognostic impact on complete remission (CR) rate or CIR. In the 104 patients who achieved CR, post-induction WT1 MRD level was predictive of relapse: 18-month CIR was 70% (95%CI: [49% - 84%]) in poor responders (n=31) versus 38% [26% - 50%] in good responders (n=73) (p=0.0001). When adjusted on cytogenetics, randomization arm and FLT3-ITD status, WT1 MRD remained independently associated with relapse (HR: 2.43, [1.25 – 4.75], p=0.009).
Similarly, NPM1mut transcript levels at diagnosis had no prognostic impact on CR rate or CIR. Among the 67 NPM1mut patients who achieved CR, post-induction NPM1mut MRD level was predictive of relapse: 18-month CIR was 64% [45% – 70%] in poor responders (n=50) versus 25% [10% – 42%] in good responders (n=17) (p=0.0007). When adjusted on randomization arm and FLT3-ITD status, NPM1 MRD remained independently associated with relapse (HR: 4.2, [1.2 – 14.3], p=0.02).
We were able to evaluate both MRD markers in 53 patients after induction (NPM1+/WT1+ n=16, NPM1+/WT1- n=24, NPM1-/WT1- n= 13). 18-month CIR was significantly different in the 3 groups (respectively 69% [38% - 87%], 40% [19% - 60%] and 25% [5% - 51%], p=0.008). In patients with poor MRD response assessed by NPM1mut, the presence of a positive WT1 MRD level was associated with a higher CIR.
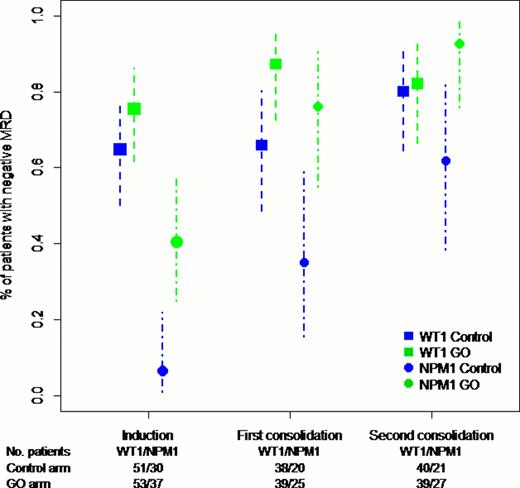
NPM1 MRD good response was more frequently observed in GO arm as compared to control arm (OR: 4.38 [2.12 – 9.03], p<0.0001). The rate of good NPM1 MRD response was 41% versus 7% after induction, 76% versus 35% and 93% versus 62% after first and second consolidation in GO and control arms respectively. WT1 MRD good response was more frequently observed in GO arm, although not reaching statistical significance (OR: 1.84 [0.89 – 3.77] p=0.098). The rate of good WT1 MRD response was 76% versus 65% after induction, 87% versus 66% and 87% versus 80% after first and second consolidation, respectively in GO and in control arms (figure 1).
Our study confirms the predictive value of MRD based on NPM1 mutations and WT1 expression in patients treated in the ALFA 0701 randomized trial. In multivariate analysis, WT1 and NPM1 MRD levels remained independent prognostic factors for relapse. We showed that treatment with GO significantly improved MRD response in adult AML.
Castaigne:Wyeth: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal