Abstract
Abstract  591
591
Survival of patients with MM has improved over the past two decades, in part due to the use of AHCT. Increasingly, second primary malignancies (SPMs) are observed in MM survivors. Determining the baseline incidence and risk factors associated with SPMs after AHCT is important to assess risk and to evaluate the risk-benefit ratio of newer therapies.
We analyzed the incidence of SPMs in 3784 MM patients receiving (“upfront”) AHCT for MM within 18 months of diagnosis between 1990 and 2010 and reported to the CIBMTR. Cumulative incidence rates of SPMs were estimated taking into account the competing risk of death. For each transplant recipient, the number of person-years at risk was calculated from the date of transplantation until date of last contact, death, or diagnosis of SPM, whichever occurred first. Incidence rates for all invasive cancers in the general population were obtained from the SEER database. Age-, sex-, and race- specific incidence rates for overall SPMs and particular anatomical sites were applied to the appropriate person-years at risk to compute the expected numbers of cancers. Observed–to –expected (O/E) ratios were calculated, and Poisson distribution 99% confidence intervals (CIs) were generated. Poisson regression model was used to analyze risk factors for overall SPMs and AML/MDS.
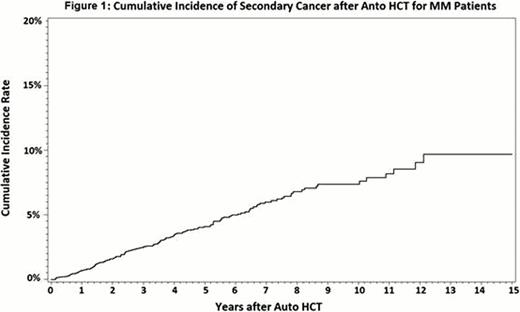
Pre-transplant therapy included novel agents in 56% including thalidomide (35%), lenalidomide (9%), bortezomib (16%) or their combinations (11%). Majority (80%) received high dose melphalan conditioning. Post-transplant maintenance therapy included thalidomide (16%), lenalidomide (8%), bortezomib (9%) and interferon (6%). Median follow-up of survivors was 52 months (range 3 to 192 months).With 12707 person years of follow up, 153 new malignancies were reported with a crude rate of 1.2 SPM per 100 person years of follow up. Observed/Expected [O/E] ratio for all SPMs was 0.99 (99% CI, 0.80–1.22). Cumulative incidence of SPM overall was 2.48% (95% CI, 1.96–3.05) at 3 years and 6.0% (95% CI, 4.96–7.10) at 7 years [Figure 1]. Individual SPMs observed significantly more frequently than expected are summarized in Table 1.
The cumulative incidence of MDS/AML was 0.5% (95% CI, 0.28–0.78) at 3 years and 1.3 (95% CI, 0.85– 1.9%) at 7 years. Majority had MM progression prior to diagnosis of SPM (65 of 102 patients overall and 15 of 23 patients for MDS/AML).
In multivariate analysis, significant risk factors for development of SPMs included: obesity [Hazard ratio = HR 1.89(95%CI, 1.21–2.93), p=0.0047 for BMI>30 vs. BMI<25], older age: [HR10.53 (95%CI, 1.46–75.82), p=0.0195] for 60–69 year olds and HR14.4 (95%CI, 1.89–109.75), p=0.01 for 70+ year olds compared to the 18–39 year old group. Specific conditioning regimens did not correlate with the risk of SPM.
The low number of MDS/AML (33 events out of 3784 cases) limited the power of multivariate analysis. Increasing age was significantly associated with development of MDS (HR10.77, (95%CI,92.09–55.51), p=0.004 for 70+ year old vs. 40–49 year olds).
In this large cohort of AHCT recipients for MM, the incidence of MDS/AML, melanoma and other skin cancers was significantly higher compared to age and sex matched general population. However the overall risk of SPM was similar to that expected for age and sex matched population. It was also similar to the placebo arms of recent reports by McCarthy Pl et al and Attal M et al (N Engl J Med. 10; 366(19):1770–91). Lenalidomide (8%) or thalidomide maintenance (16%) used in a small subset of patients with comparatively short follow up, was not associated with risk of SPM in the analysis of the overall cohort.
| Ratio of observed to expected (O/E) cases of SPM at various time periods post AHCT and 99% confidence intervals. . | ||||
|---|---|---|---|---|
| Time period . | 2-5 years . | 5-10 years . | 10-20 years . | Overall . |
| Person-Years at risk | 4502 | 1769 | 158 | 12707 |
| All SPM | 1.03 (0.71–1.43) | 1.38 (0.84–2.11) | 2.41 (0.62–6.29) | 0.99 (0.80–1.22) |
| MDS | 105.63 (43.51–212.54) | 109.70 (28.10–286.30) | 172.88 (0.86–1284.51) | 85.52 (48.48–138.97) |
| AML | 7.45 (1.25–23.45) | 8.28 (0.43–38.41) | 83.14 (4.30–385.50) | 5.48 (1.76–12.73) |
| Melanoma | 1.65 (0.19–6.03) | 3.80 (0.43–13.91) | 14.12 (0.07–104.93) | 3.37 (1.63–6.1) |
| Other skin cancers | 29.39 (4.94–92.54) | 81.32 (17.62–231.30) | None | 37.76 (16.8–72.37) |
| Ratio of observed to expected (O/E) cases of SPM at various time periods post AHCT and 99% confidence intervals. . | ||||
|---|---|---|---|---|
| Time period . | 2-5 years . | 5-10 years . | 10-20 years . | Overall . |
| Person-Years at risk | 4502 | 1769 | 158 | 12707 |
| All SPM | 1.03 (0.71–1.43) | 1.38 (0.84–2.11) | 2.41 (0.62–6.29) | 0.99 (0.80–1.22) |
| MDS | 105.63 (43.51–212.54) | 109.70 (28.10–286.30) | 172.88 (0.86–1284.51) | 85.52 (48.48–138.97) |
| AML | 7.45 (1.25–23.45) | 8.28 (0.43–38.41) | 83.14 (4.30–385.50) | 5.48 (1.76–12.73) |
| Melanoma | 1.65 (0.19–6.03) | 3.80 (0.43–13.91) | 14.12 (0.07–104.93) | 3.37 (1.63–6.1) |
| Other skin cancers | 29.39 (4.94–92.54) | 81.32 (17.62–231.30) | None | 37.76 (16.8–72.37) |
Gale:Celgene: Employment. Brandenburg:Celgene: Employment, Equity Ownership. Lonial:Millennium, Celgene, Novartis, BMS, Onyx, Merck all Consultancy. Krishnan:Celgene and Millennium: Consultancy, Speakers Bureau. Dispenzieri:Celgene and Millennium: Research Funding. Hari:Celgene: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal