Abstract
Abstract 5182
The 1-yr open-label, single-arm, multicenter EPIC (Evaluation of Patients' Iron Chelation with Exjade®) trial assessed the efficacy and safety of deferasirox in patients with transfusion-dependent iron overload, including patients with thalassemia and with myelodysplastic syndromes (MDS). The most frequent adverse events (AEs) in the EPIC trial were gastrointestinal (GI) disturbances. Here, we qualitatively examine concomitant medication (con med) use in thalassemia and MDS patients with/without GI events to consider the impact of con med use on GI events.
Thalassemia and MDS patients from the EPIC study were included. A GI event was defined as an investigator-reported AE with the system organ class ‘GI disorders’ after start of treatment. Data are reported here for the most frequently received con meds of interest, by preferred term, which also had notable differences in their frequency among patients with/without GI events; con meds that may have been prescribed to treat GI events are excluded from interpretation: propulsives, antipropulsives, proton pump inhibitors, laxatives and electrolyte solutions.
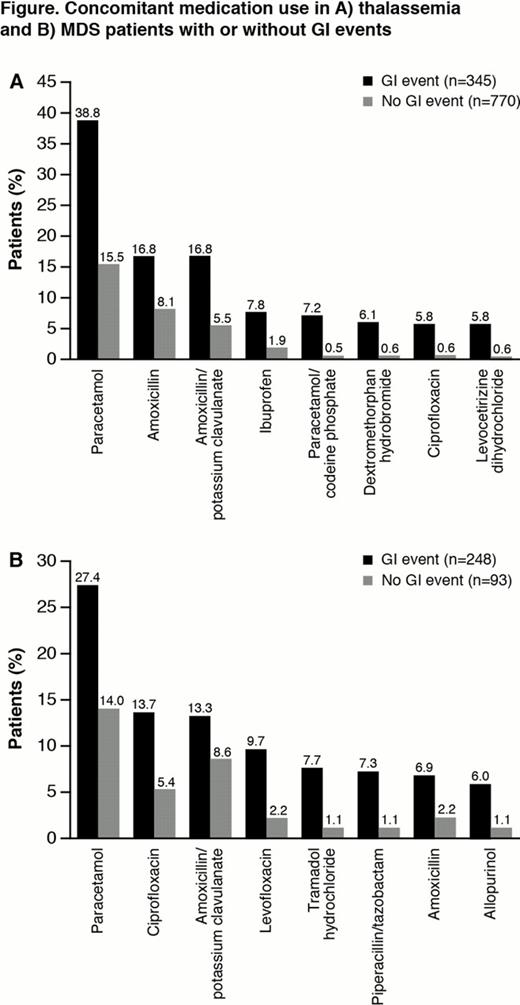
Among thalassemia patients (n=1115; 48. 3% male; aged 18. 2 yrs [range 2–72]), 345 (30. 9%) patients experienced a GI event. Mean deferasirox dose was 23. 8 ± 5. 4 mg/kg/d in patients with a GI event and 24. 3 ± 5. 5 mg/kg/d in patients with no GI event; median serum ferritin (SF) at end of study (EOS) was 2734 ng/mL (391–23997) and 3223 ng/mL (259–17644), respectively. 28. 9% of thalassemia patients did not receive any con meds; 15. 7% received ≥7 different types of con meds. Thalassemia patients with a GI event received a mean of 6. 0 different types of con meds, vs 2. 1 in patients without a GI event. Con meds were received in 91. 9% of patients with a GI event vs 61. 8% of patients without a GI event. Anti-inflammatory, antibiotic or antifungal con meds were more frequent in thalassemia patients who experienced a GI event (Figure A). The con med with the largest relative difference in frequency among patients with vs without a GI event was paracetamol/codeine phosphate (7. 2 vs 0. 5%, respectively).
Among MDS patients (n=341; 59. 8% male; aged 67. 9 yrs [11–89]), 248 (72. 7%) patients experienced a GI event. Deferasirox dose was 18. 8 ± 4. 9 mg/kg/d in patients with a GI event and 20. 4 ± 6. 4 mg/kg/d in patients with no GI event; SF at EOS was 1977 ng/mL (254–9835) and 2045 ng/mL (141–10155), respectively. 12. 3% of MDS patients did not receive any con meds; 37. 8% received ≥7 different types. Patients with a GI event received a mean of 9. 6 different types of con meds vs 4. 5 in patients without a GI event. Con meds were received in 89. 5% of patients with a GI event, vs 82. 8% of patients without a GI event. In patients with MDS, antibiotic, antifungal or opioid medications were more frequent in patients with GI events (Figure B). The con med with the largest relative difference in frequency among patients with vs without a GI event was tramadol hydrochloride (7. 7 vs 1. 1%, respectively).
Most frequent con med in both populations was paracetamol (acetaminophen; Figure). In patients receiving paracetamol who had a GI event, the most frequent types of GI events in thalassemia patients were diarrhea, abdominal pain and nausea; in MDS patients these were diarrhea, constipation and abdominal pain. In patients receiving paracetamol, mean alanine aminotransferase level at EOS in thalassemia patients with a GI event was 49. 0 vs 46. 3 U/L in patients with no GI event; and 38. 9 vs 27. 2 U/L in MDS patients, respectively.
In both thalassemia and MDS patients, concomitant use of antifungal and antibiotic medications was more frequent in patients with GI events, although it should be considered that GI events are also the most frequent AEs of, for eg, amoxicillin/potassium clavulanate and ciprofloxacin. Paracetamol use was higher in patients who had GI events; types of GI events were typical of those observed during deferasirox treatment and did not appear related to liver toxicity. Anti-inflammatory medications were more frequent in thalassemia patients with GI events, as were opioid medications in MDS patients. Con meds may affect the frequency of GI AEs reported with deferasirox. Further investigation is needed to determine whether these observations result from a potential interaction of the metabolic pathways of con meds and deferasirox – eg, CYP450 metabolism of paracetamol – or the action of the con meds alone.
Cappellini:Novartis: Speakers Bureau. Porter:Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Kattamis:Novartis: Honoraria, Research Funding, Speakers Bureau. Louw:Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. El-Ali:Novartis: Employment. Martin:Novartis: Employment. Gattermann:Novartis: Honoraria, Research Funding, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal