Abstract
Abstract 5124
Acute lymphoblastic leukemia (ALL) is a complex genetic disease involving many fusion oncogenes (FGs) (Xu et al., 2012). The frequency of various FO can vary in different ethnic groups & these FGs have important implications for prognosis & treatment outcome (van-Dongen et al, 1999).
We studied FGs in 101 pediatric ALL patients using Interphase FISH & RT-PCR (van-Dongen et al, 1999), & their association with clinical features & treatment outcome.
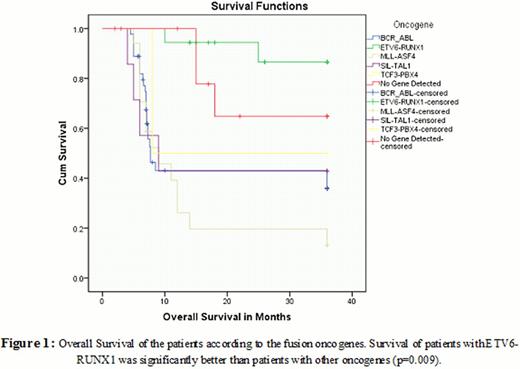
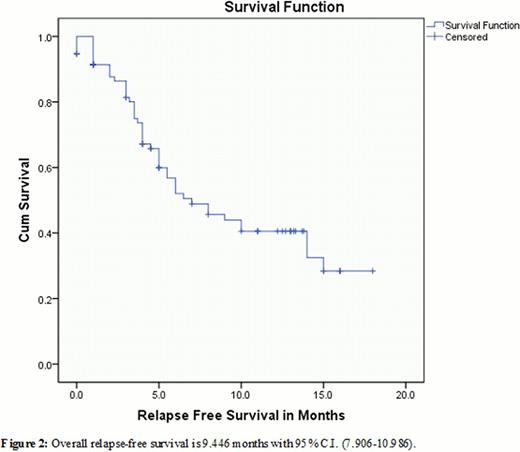
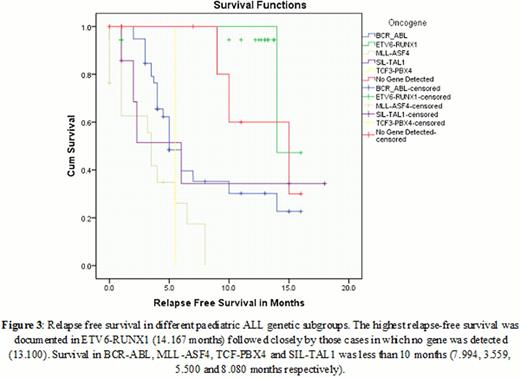
Five most common FGs i. e. BCR-ABL [t(9;22)], TCF3-PBX1 [t(1;19)], ETV6-RUNX1 [t(12;21)], MLL-AF4 [t(4;11)] & SIL-TAL1 (del 1p32) were found in 89/101 (88. 1%) patients. Frequency of BCR-ABL was 44. 5% (45/101) (Table 1). BCR-ABL positive patients had a significantly lower survival (43. 73 ± 4. 24 weeks) (Figure 1)& higher white cell count as compared to others except patients with MLL-AF4. The highest relapse-free survival (RFS) was documented in ETV6-RUNX1 (14. 167 months) followed closely by those cases in which no gene was detected (13/100). RFS in BCR-ABL, MLL-ASF4, TCF-PBX4 & SIL-TAL1 was less than 10 months (7. 994, 3. 559, 5. 500 & 8. 080 months respectively) (Figure 2 & 3).
Frequency of occurrence was directly proportional to age (3 less than 2 year age group, 16 in the 2–7 year age group & 26 in the older than 7 group. Total leukocyte count (TLC) was higher when compared to patients with other oncogenes. Organomegaly was not common. BCR-ABL positivity was associated with low remission rates & shortened survival.
The median age of the patients was 1. 85 years. The gene frequency was highest in patients younger than 2 years. TLC was not very high & patients had a good prognosis.
17 patients had MLL-AF4 gene rearrangement with a median age of 9 years. Five patients were younger than 2 years, two between 2 & 7 years, & ten patients were in the 7–15 age group. Majority of our patients were older unlike the usual occurrence where most of the patients are infants.
This FG occurs in around 2% of patients. Only two female patients were diagnosed with this translocation. Both the patients were over 2 years of age. It was associated with an inferior outcome in the context of response to chemotherapy & a higher risk of CNS relapse although small numbers preclude any firm conclusions.
Patients were older than 2 years, with the majority falling in the age range 7 to 15 years. The immunophenotype data were available in all SIL-TAL1 patients showing this fusion gene was associated with T-ALL with organomegaly being observed frequently.
This is the first study from Pakistan correlating molecular markers with disease biology & treatment outcome in pediatric ALL. Our study revealed the highest reported frequency of BCR-ABL FO in pediatric ALL, in consistent with various other reports from Pakistan & rest of the world ((Iqbal & Akhtar, 2007; Faiz et al., 2011; (Gaynon et al., 1997; Iacobucci et al., 2012).) which, consequently, was associated with poor overall survival. The data indicates an immediate need for incorporation of tyrosine kinase inhibitors in the treatment of BCR-ABL+ pediatric ALL in this population & the development of facilities for stem cell transplantation.
Comparison of clinical characteristic of pediatric ALL patients
| Clinical & laboratory parameters . | BCR-ABL No (%) N=45 . | ETV6-RUNX1 No (%) N=18 . | MLL-AF4 No (%) N=17 . | SIL-TAL1 No (%) N=7 . | TCF3-PBX1 No (%) N=2 . | FO not detected No (%) N=12 . |
|---|---|---|---|---|---|---|
| Male | 34 (75) | 11 (61) | 12 (70.5) | 3 (42.8) | 0 | 9 (75) |
| Female | 11 (24.4) | 7 (38.8) | 5 (29.4) | 4 (57.1) | 2 (100) | 3 (25) |
| Age | ||||||
| <2 | 3 (6.7) | 10 (55.5) | 5 (29.4) | 0 | 0 | 0 |
| 2-7 | 16 (35.6) | 7 (38.8) | 2 (11.8) | 2 (28.6) | 1 (50) | 5 (41.6) |
| 8-15 | 26 (57.8) | 1 (5.5) | 10 (58.8) | 5 (71.4) | 1 (50) | 7 (58.4) |
| WBC | ||||||
| <30,000 | 24 (53.3) | 17 (94.4) | 10 (58.8) | 4 (57.1) | 1 (50) | 9 (75) |
| >30,000 | 21 (46.6) | 1 (5.5) | 7 (41.1) | 3 (42.8) | 1 (50) | 3 (25) |
| Hepatomegaly | ||||||
| No | 23 (51.1) | 15 (83.3) | 8 (47.1) | 3 (42.9) | 0 | 9 (12) |
| Yes | 22 (48.9) | 3 (16.7) | 9 (53) | 4 (57.1) | 2 (100) | 3 (25) |
| Splenomegaly | ||||||
| No | 35 (77.8) | 15 (83.3) | 9 (53) | 5 (71.4) | 0 | 7 (58.3) |
| Yes | 10 (23.3) | 3 (17.7) | 8 (47.1) | 2 (28.6) | 2 (100) | 5 (41.7) |
| Lymphadenopathy | ||||||
| No | 30 (66.7) | 11 (61.1) | 5 (29.4) | 5 (21) | 2 (100) | 0 |
| Yes | 15 (33.3) | 7 (38.9) | 12 (70.6) | 2 (28) | 0 | 2 (16.7) |
| Platelets | ||||||
| <50,000 | 14 (31.1) | 6 (33.3) | 9 (52.9) | 6 (85.7) | 2 (100) | 3 (25) |
| >50,000 | 31 (68.9) | 12 (66.7) | 8 (47.1) | 1 (14.7) | 0 | 9 (75) |
| CR | ||||||
| <4weeks | 13 (28.9) | 16 (94.4) | 4 (23.5) | 5 (71.4) | 1 (50) | 8 (66.7) |
| >4weeks | 29 (64.4) | 1 (5.6) | 10 (82.4) | 1 (14.2) | 1 (50) | 2 (16.6) |
| No remission | 3 (6.7) | 1 (5.6) | 3 (13.6) | 1 (14.2) | 0 | 2 (16.6) |
| Clinical & laboratory parameters . | BCR-ABL No (%) N=45 . | ETV6-RUNX1 No (%) N=18 . | MLL-AF4 No (%) N=17 . | SIL-TAL1 No (%) N=7 . | TCF3-PBX1 No (%) N=2 . | FO not detected No (%) N=12 . |
|---|---|---|---|---|---|---|
| Male | 34 (75) | 11 (61) | 12 (70.5) | 3 (42.8) | 0 | 9 (75) |
| Female | 11 (24.4) | 7 (38.8) | 5 (29.4) | 4 (57.1) | 2 (100) | 3 (25) |
| Age | ||||||
| <2 | 3 (6.7) | 10 (55.5) | 5 (29.4) | 0 | 0 | 0 |
| 2-7 | 16 (35.6) | 7 (38.8) | 2 (11.8) | 2 (28.6) | 1 (50) | 5 (41.6) |
| 8-15 | 26 (57.8) | 1 (5.5) | 10 (58.8) | 5 (71.4) | 1 (50) | 7 (58.4) |
| WBC | ||||||
| <30,000 | 24 (53.3) | 17 (94.4) | 10 (58.8) | 4 (57.1) | 1 (50) | 9 (75) |
| >30,000 | 21 (46.6) | 1 (5.5) | 7 (41.1) | 3 (42.8) | 1 (50) | 3 (25) |
| Hepatomegaly | ||||||
| No | 23 (51.1) | 15 (83.3) | 8 (47.1) | 3 (42.9) | 0 | 9 (12) |
| Yes | 22 (48.9) | 3 (16.7) | 9 (53) | 4 (57.1) | 2 (100) | 3 (25) |
| Splenomegaly | ||||||
| No | 35 (77.8) | 15 (83.3) | 9 (53) | 5 (71.4) | 0 | 7 (58.3) |
| Yes | 10 (23.3) | 3 (17.7) | 8 (47.1) | 2 (28.6) | 2 (100) | 5 (41.7) |
| Lymphadenopathy | ||||||
| No | 30 (66.7) | 11 (61.1) | 5 (29.4) | 5 (21) | 2 (100) | 0 |
| Yes | 15 (33.3) | 7 (38.9) | 12 (70.6) | 2 (28) | 0 | 2 (16.7) |
| Platelets | ||||||
| <50,000 | 14 (31.1) | 6 (33.3) | 9 (52.9) | 6 (85.7) | 2 (100) | 3 (25) |
| >50,000 | 31 (68.9) | 12 (66.7) | 8 (47.1) | 1 (14.7) | 0 | 9 (75) |
| CR | ||||||
| <4weeks | 13 (28.9) | 16 (94.4) | 4 (23.5) | 5 (71.4) | 1 (50) | 8 (66.7) |
| >4weeks | 29 (64.4) | 1 (5.6) | 10 (82.4) | 1 (14.2) | 1 (50) | 2 (16.6) |
| No remission | 3 (6.7) | 1 (5.6) | 3 (13.6) | 1 (14.2) | 0 | 2 (16.6) |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal