Abstract
Abstract 4960
MDS ‘s clinical pathology is heterogeneous such as the intensity of cytopenia and the rate and the timing of AML evolution. The definite algorithm is difficult to be settled. We have several approved agents as the MDS therapy in Japan, Thalidomide, Lenalidomide and 5-Azacytidine (AZA) in addition to the conventional agents such as immunosuppressive agents (predonisolone and cyclospoline-A) and hematopoietic cytokines (G-CSF, Erythropoietin). We retrospectively analyze 36 MDS patients who were treated since 2004 in our hospital. The first current treatment was the conventional agents and transfusion that we call best supportive care (BSC). Since 2006 we could treat by thalidomide in addition to the conventional ones. Lenalidomide is limited to use only for 5q- MDS that is not included in 36 MDS. It was 2011 that we applied stem cell transplantation (SCT) for AML/MDS (AML evoluted from MDS). This conditioning regimen is low dose or non-myeloablative that is feasible to older individuals. The stem cell source of haploidentical donor or cord blood is immediately available at the time of urgent transplantation. The rate of GVHD of these HLA-mismatch transplantations is not so high as generally thought. The optimal SCT timing is very difficult and important.
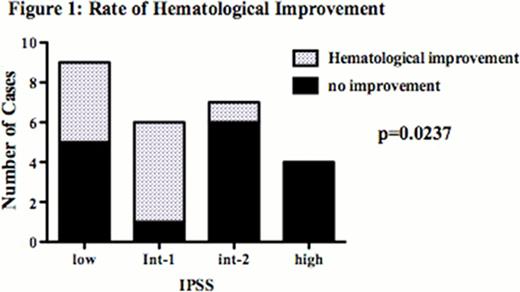
In the baseline characteristics of consecutive 36 MDS patients, the median age was 70 (range 39 ∼ 90), F/M was 24/12. The 26 of them were treated by thalidomide daily 50mg∼100mg as the first line therapy, whose diagnosis was RCUD n=6, RARS n=2, RCMD n=9, RAEB-1 n=2 RAEB-2 n=4 and AML/MDS n=3. Using IPSS score, there were 9 patients with low, 6 int-1, 7 int-2 and 4 high (including 3 AML/MDS). 8 int-2 and 1 high had complex karyotype that is cytogenetically high risk. The other 8 patients received the best supportive care (BSC) by immunosuppressive agents, cytokines and transfusion. Two another patients were treated by AZA as the first line. Two of three AML/MDS had received stem cell transplantation (62 years male received haplo-mini SCT and 75 years female received cord blood SCT).
Thalidomide produced hematological improvement in 70% of lower IPSS (low and int-1) simultaneously with transfusion independency. On the contrary, int-2 improved only in 14%, high and AML/MDS in 0% (Fig 1). The improvement by thalidomide of RARS was 100% and RCMD was 67%. The p value about the improvement about WHO classification was 0. 182 because of the insufficiency of the number of patients. When the over all survival of thalidomide treated patients is compared with BSC patients, there was no statistically difference between them in lower risk MDS. In higher risk MDS, two int-2 patients who had failed with the single use of thalidomide achieved the hematological improvement by the combination of thalidomide and AZA. One of them was cytogenetically high risk. Their AZA cycles were 14 and 12. They were still receiving AZA. After the long-term follow-up, it will be clear that this combination makes statistical predominant in OS. This combination was completely ineffective against AML/MDS who received stem cell transplantation as second-line therapy. After the transplantation they received AZA maintenance that is expected to suppress minimal residual disease while monitoring WT1 expression. They are alive now for 1. 41 and 1. 01 years since they were diagnosed as AML/MDS.
Thalidomide makes good hematological response of lower risk MDS and bring the free of transfusion that elevates and maintains the QOL of the patients. About the higher risk of MDS, thalidomide single therapy has no works but its' combination with AZA is very effective and bring not only the hematological improvement but also the possibility of longer overall survival. For AML/MDS, stem cell transplantation is the only potential curative treatment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal