Abstract
Abstract 4887
Chronic active Epstein-Barr virus infection (CAEBV) has been implicated in several diseases including hemophagocytic lymphohistiocytosis (EBV-HLH) and lymphomas including Angioimmunoblastic T cell lymphoma. The exact mechanism by which EBV infection causes these complications is currently not well understood. EBV-HLH is a syndrome in which T-cells, NK cells and macrophages are aberrantly activated. Cytokine storms play a major role in cellular damage and organ dysfunction. In the event that the body is unable to clear the EBV viremia, dysregulated T, NK cells and macrophages continue to release cytokines leading to the accumulation of lymphohistiocytic infiltrates into organs and organ damage. Cytokine storms can lead to death from multi-organ failure. During a cytokine storm, levels of several cytokines are elevated including TNF-a, IFN-g, sCD25, IL-12, IL-1, IL-10 and IL-18.1–3 Current lines of therapy of EBV-HLH include steroids, etoposide, cyclosporine, ATG and hematopoietic stem cell transplantation. We report successfully controlling frequent cytokine storms in a patient with EBV induced angioimmunoblastic lymphoma and HLH with weekly infliximab after failure to do so with chemotherapy (CHOP-E; cyclophosphamide, daunorubicin, vincristine, prednisone, etoposide), rituximab and bortezomib.
This is a 35 year old African American male with a long history of adenopathy who presented with autoimmune hemolytic anemia, autoimmune thrombocytopenia (ITP), neutropenia with fever and hypotension. Work up revealed persistent EBV viremia and the lymph node biopsy revealed Angioimmunoblastic T cell lymphoma. High dose dexamethasone and Intravenous immunoglobulins (IVIG) failed to control his hemolysis and ITP. Rituximab and bortezomib successfully controlled his autoimmune hemolysis and thrombocytopenia. However, cytokine storm episodes, characterized by high fevers, hypotension and respiratory distress, continued every 1–2 weeks requiring ICU admissions. Chemotherapy (CHOP-E), for his underlying lymphoma, followed by etoposide/steroids (HLH-94 protocol) were also ineffective at controlling his cytokine storms. Considering that he had high levels of TNF-a, infliximab was started in an attempt to control dysregulated macrophages and T-cells, and was able to successfully prevent the cytokine storms. High levels of IL-6, soluble IL-2 receptor and TNF-a were all detected during cytokine storm episodes. The patient is currently getting prepared for an allogeneic stem cell transplant.
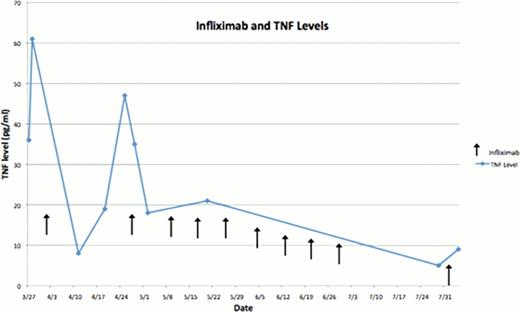
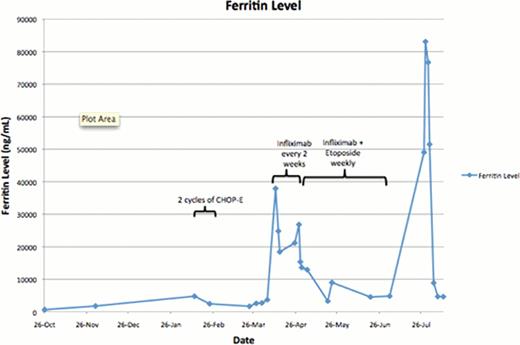
We report successful control of EBV-HLH related cytokine storms, guided by TNF-a levels, with weekly infliximab (Fig 1). Hypercytokinemia is believed to result from dysregulated T cells, NK cells and macrophages as a result of failure to control the EBV viremia. In this case a TNF-a inhibitor (infliximab) was used to control dysregulated macrophages, T and NK cells and block further propagation of inflammatory cytokines. Initially infliximab was initiated on a once every 2 week schedule, however, this failed to prevent cytokine storms with high TNF-a levels. However, weekly dosing of infliximab successfully prevented cytokine storms and controlled his TNF-a levels (Fig 1). Moreover, an attempt to taper off the weekly infliximab and etoposide resulted in relapse of his symptoms and a sharp rise in ferritin levels, a marker for HLH activity (Fig 2). This suggests that infliximab might be an effective therapy in preventing cytokine storms related to EBV-HLH and further studies are warranted.
Elevated levels of TNF-a Levels were successfully controlled with weekly infliximab which correlated with clinical improvement and prevention of cytokine storms
Elevated levels of TNF-a Levels were successfully controlled with weekly infliximab which correlated with clinical improvement and prevention of cytokine storms
Ferritin levels were used to monitor the activity of the hemophagocytic syndrome. After initiation of weekly infliximab, guided by TNF-a levels, the ferritin level remained low with clinical improvement. A trial of tapering the infliximab and etoposide resulted in a relapse of symptoms and a sharp rise in ferritin level.
Ferritin levels were used to monitor the activity of the hemophagocytic syndrome. After initiation of weekly infliximab, guided by TNF-a levels, the ferritin level remained low with clinical improvement. A trial of tapering the infliximab and etoposide resulted in a relapse of symptoms and a sharp rise in ferritin level.
Besa:Celgene: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal