Abstract
Abstract 4732
Bone defection repairing is a good model to study the hematopoiesis and its environment, during which there are reformations of niches and marrow cavity, different cells' migrations and evolutions, etc. Tissue-engineering-bone (TEB) is a kind of scaffold that degrades gradually during bone reformation. In order to observe different cells growing within the rigid, opaque, friable and porous TEB, we established a novel technique named semi-solid decalcification (SSD).
With the TEB repairing model, we hope to address 3 questions: Firstly, could a functional bone with marrow cavity be reformed with the TEB? Secondly, what are the contributions of cells within and outside the TEB? Thirdly, how do the hematopoietic cells cross-talking with the microenvironment during bone reformation?
GFP+ mesenchymal cells were isolated from GFP transgenic FVB mice, expanded/purified with a murine MSC kit (cat no. MUCMX-90011, Saiye Company, China).
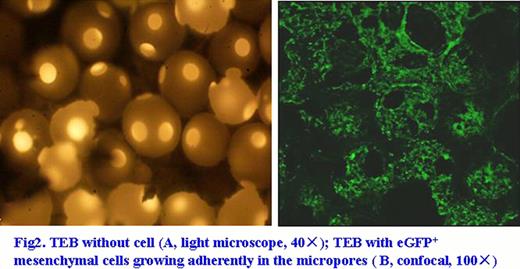
TEB b-TCP scaffold (3mm × 5mm, with microtubule pleural furrow, Bio-lu Company, France) was preloaded with 6th passage of eGFP mesenchymal cells (TEB-MC-GFP) 2d before implantation.
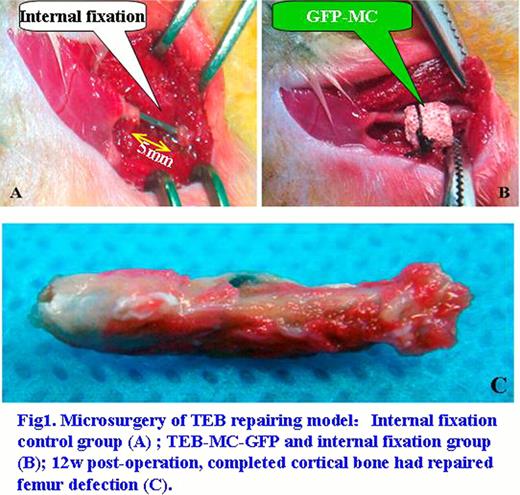
Five mRFP transgenic FVB mice were made segmental femur resects (5mm, half of femur length) by microsurgery, then 2 with internal fixation only as control, 3 were implanted with TEB-MC-GFP and internal fixation (Fig 1a, 1b).
Bone formation throughout the defects was assessed radio graphically 4, 8 and 12w after the implantation.
Total body paraformaldehyde perfusion fixation was performed 12w after, and then samples of different organs were collected for frozen sections except the femur, while the femur underwent SSD before observation under confocal microscope and further frozen section.
Samples from different parts of the femurs were taken under invert fluorescence microscope after SSD, for detecting GFP and cytokines gene expression by RQ-PCR, ABL as control gene.
X-ray shows the internal fixation is reliable and 5mm bone defects could not self-cure without TEB.
Completed cortical bone has covered the TEB repairing femur defects 12w after operation (Fig 1c).
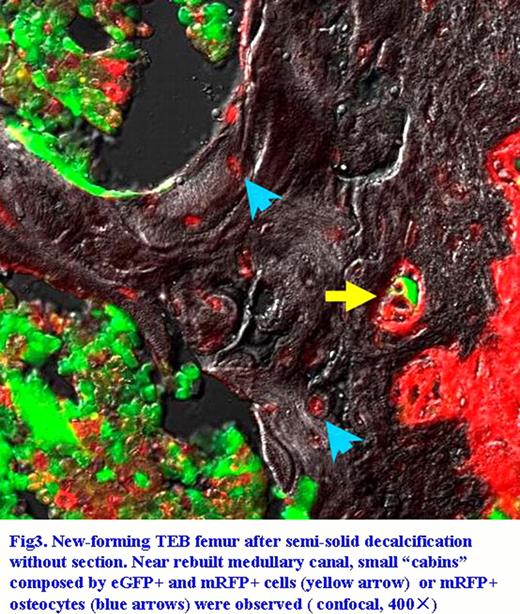
Observing the frozen section under confocal microscope after SSD shows that: (a) eGFP+ mesenchymal cells grow adherently inside the pores of the TEB before implantation (Fig 2a, 2b). (b) New cartilage and bone tissues had been formed, many eGFP+ and mRFP+ cells growing together in the pores of relic scaffold, new-forming collagen with red fluorescence inserting into the pores of TEB. To our surprising, eGFP+ cells are the majority component of marrow cavity. (c) Near rebuilt medullary canal, small “cabins” composed by eGFP+ and/or mRFP+ cells can been clearly observed, synapses and hairs of cells can be distinguished (Fig 3). (d) Middle or small blood vessels around and within the TEB were constructed by mRFP+ and/or eGFP+ cells. eGFP+ cells could be found not only in muscles nearby, but also in murine kidney, lung and gut, et al.
The eGFP/ABL ratio of RQ-PCR in the middle of TEB > in the connection of TEB with normal bone > muscles nearby, which are 0.436±0.036, 0.140±0.038 and 0.098±0.024, respectively(P=0.000), in accordance with the expression of VEGF/ABL (P=0.003).
This eGFP-to-mRFP transgenic mice femur repairing model was proved, at least in principle, to be efficient to mimic the reforming of bone marrow and stem cell niche. With the help of SSD, we can easily study the relationship and cross-talking of cell-cell and cell-matrix in a 3-D pattern, which is of the most important to understand the mechanism of hematopoiesis microenvironment. However, further researches are carrying on, to exclude the possible mixture of eGFP+ hematopoietic cells into mesenchymal cells before TEB-MC-GFP implantation and to better identify the subtypes of existing cells within the TEB.
PS: Thanks to the support of NSFC (No.30901367, 31070866).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal