Abstract
Abstract 4285
The prognostic value of geriatric assessment variables in older adults with acute myelogenous leukemia (AML) is not known.
To determine the relation between baseline geriatric assessment and survival in older patients with AML.
We aimed to prospectively enroll all consecutive patients with AML ≥ 65 years of age who presented to Dana-Farber Cancer Institute between 2006–2011. Patients completed the EORTC-30 quality of life questionnaire at their initial visit, prior to receiving chemotherapy. We evaluated questions corresponding to geriatric domains including physical, social and cognitive functions, psychological state, nutrition and pain. We extracted patient demographics and clinico-pathologic data from medical records. Baseline Comorbidity score was calculated using the Hematopoietic Stem Cell Transplant Comorbidity Index (HCT-CI). We used Kaplan-Meier and Cox proportional hazards models to estimate survival.
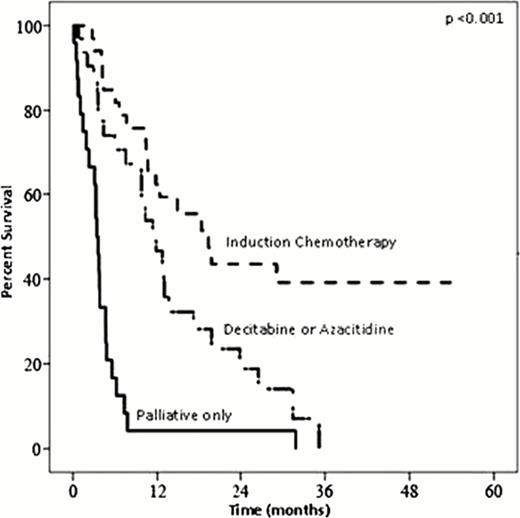
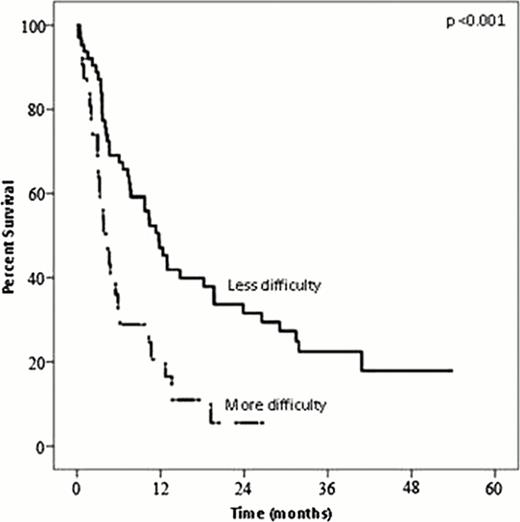
101 patients with AML ≥ 65 consented to be followed and were available for analysis. Median age was 72 years (range: 65–90) and most patients were white (98%), male (62%) and had a performance status of 1 or less (79%). Only 38% of patients had more than one comorbidity, and only 3 patients required help with activities of daily living. The majority of patients (78%) received treatment. Of those treated, 45% underwent induction chemotherapy and 44% received decitabine or azacitidine. The one-year overall survival of the group was 37.4 % ±5.0% and the one-year disease-specific survival (DSS) was 39.0 % ±5.1%. Survival varied substantially based on treatment type (Figure 1). Self-reported difficulty with strenuous activity (Figure 2) and presence of pain were associated with decreased survival. On multivariate analysis, age at diagnosis >72 years vs. ≤ 72 years (Hazard Ratio [HR]=1.75; 95%CI 1.05 to 2.91), cytogenetic risk group (adverse vs. intermediate and favorable); HR=1.99; 95% CI 1.21 to 3.26), secondary vs. de novo AML (HR=1.61; 95% CI 1.00 to 2.62), comorbidity score >1 vs. ≤1 (HR=1.84; 95%CI 1.10 to 3.07), more vs. less difficulty with strenuous activity (HR=1.74; 95%CI 1.05 to 2.89), and pain more vs. less often (HR=2.16; 95% CI 1.17 to 3.98) were independent prognostic factors for worse survival. When we limited the analysis to the 80 patients with ECOG PS ≤1, difficulty with strenuous activities, pain, and comorbidity remained independent predictors for survival.
In this highly selected population of older patients with AML, we found that geriatric assessment variables were independent prognostic factors for survival, even among patients with the best performance status. Our results support the use of geriatric assessment to more accurately predict prognosis in the older AML patient population.
Kaplan-Meier Plot of Survival by Difficulty with Strenuous Activity
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal