Abstract
Abstract 3887
Potassium (K)-channels play an important role in regulating cell proliferation by maintenance of the membrane potential and subsequent Ca2+ signaling. Out of 80 known human K-channel genes only the voltage gated K-channel Kv1.3 and the calcium-gated K-channel KCa3.1 are expressed in lymphocytes, with expression levels varying greatly depending on lymphocyte maturation and activation status (for review see Cahalan MD, Chandy KG, Immunol Rev. 2009). Accordingly, proliferation of various lymphocyte subtypes can be inhibited by blockade of the respective predominant K-channel. As the modulation of K-channel expression on malignantly transformed lymphocytes and their potential as therapeutic targets has been largely overlooked, we characterized the expression and function of Kv1.3 and KCa3.1 in Chronic Lymphocytic Leukemia (CLL).
Primary cells from unselected CLL-patients were isolated from peripheral blood mononuclear cells (PBMCs). Comparison of Kv1.3 and KCa3.1 levels on unstimulated CLL-cells versus PMA/ionomycin-activated CLL-cells revealed a significant reduction in the Kv1.3/KCa3.1 ratio (n=31, 1.526 vs. 0.9054, p=0.0005), as evidenced on mRNA and protein levels by RT-PCR and patch clamp analysis, respectively. Stimulation of CLL-cells with enriched and activated autologous CD4+ T-cells resulted in higher CLL-cell activation as measured by CD80/86 expression, and an even more pronounced reduction of the Kv1.3/KCa3.1 ratio. This stimulation protocol also effectively induced CLL-cell proliferation as verified by Ki-67 expression and CFSE dilution via flow cytometric measurement. Highly activated and/or proliferating CLL-cells consistently up-regulated KCa3.1 (RT-PCR: Ki-67 n=5, p=0.0013; CFSE n=5, p=0.0436; immunofluorescence (IF) staining - n=4, p=0.0121), whereas Kv1.3 was fairly low. Consistent with our in vitro data, CLL-cells in lymph node and bone marrow, believed to be primary sites of CLL-proliferation in vivo, were highly positive for KCa3.1 channels in contrast to CLL-cells from the peripheral blood as revealed by IF staining on paraffin-embedded tissue sections.
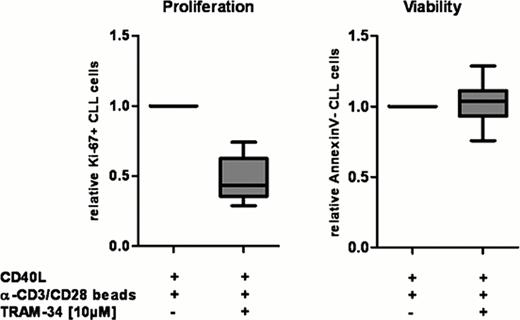
In light of the significantly increased KCa3.1-expression on activated and proliferating CLL-cells, we investigated whether specific blockade of KCa3.1 could inhibit CLL-cell proliferation. CLL-cells in PBMCs were pre-stimulated by co-culture with CD40L expressing (murine) fibroblasts for 24 hours, and were treated with highly specific blockers for KCa3.1 (TRAM-34 or Clotrimazole) or Kv1.3 (PAP-1 or Psora-4) prior to addition of α-CD3/CD28 beads to activate autologous T-cells. KCa3.1 blockade could effectively diminish CLL-cell cycle entry in all samples investigated (TRAM-34: n=12, p<0.0001; Clotrimazole: n=5, p=0.0625) with a mean relative reduction in Ki-67+ cells of 52% (SD=1.56) for TRAM-34 (see Figure left) and 53% (SD=1.11) for Clotrimazole. This antagonizing effect of TRAM-34 was clearly dose-dependent (n=10) without affecting CLL-cell viability (see Figure right) nor activation. Viability, activation and proliferation of T-cells and fibroblasts present in the co-culture system were not affected by TRAM-34. Blockade of Kv1.3 did not reduce proliferation in CLL-cells.
In summary, we showed that CLL-cells exhibit significant changes in their K-channel constitution following activation and proliferation, analogous to healthy B-cells. Notably, in vitro CLL-cell proliferation was effectively inhibited by highly specific KCa3.1 blockers. Thus far in vitro testing of potential CLL-drugs has been primarily performed on G0-arrested CLL-cells, sometimes in co-culture with stromal cells to enhance their viability. Our approach attempts to specifically target proliferating CLL-cells, presumably the most relevant CLL-cell fraction contributing to disease progression. Given their low toxicity profile, KCa3.1 blockers could represent a promising therapeutic option in CLL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal