Abstract
Abstract 3136
Follicular lymphoma (FL) is the most common indolent non-Hodgkin lymphoma (NHL) in the Western hemisphere and is likely incurable with chemotherapy alone. Despite a median overall survival exceeding 12 years in the modern era, a fraction of patients experience an aggressive clinical course characterized by short remission duration(s) and/or chemorefractory disease. While high-dose therapy and autologous stem cell rescue (HDT-ASCR) is an accepted treatment modality for prolonging progression-free survival (PFS) it is unlikely to provide cure. Allogeneic stem cell transplantation (alloSCT) is a definitive therapy that has been shown to produce long-term disease free remissions. Unfortunately, alloSCT is limited by the risk of transplant-related mortality (TRM) despite the advent of non-myeloablative (NMA) conditioning regimens. Given that many FL patients whom fail HDT-ASCR may not proceed to alloSCT, and the inherent difficulty in deciding the appropriate consolidative transplant modality, we conducted a retrospective exploratory analysis of clinical features of early and multiply relapsed FL patients undergoing first HDT-ASR or alloSCT at a single center in the modern, post-rituximab era.
We retrospectively reviewed all patients with early relapsed and/or refractory FL that proceeded to HDT-ASCR or NMA alloSCT as first transplant at MSKCC between 2006 and 2010. Chemosensitive disease was defined as a partial response (PR) or complete response (CR) to the last treatment regimen prior to transplant by computed tomography scans per IWG Criteria (Cheson et al JCO 1999). Events were defined as progression of FL post-transplant or death from any cause. Event-free survival (EFS) and overall-survival (OS) were estimated using Kaplan-Meier method.
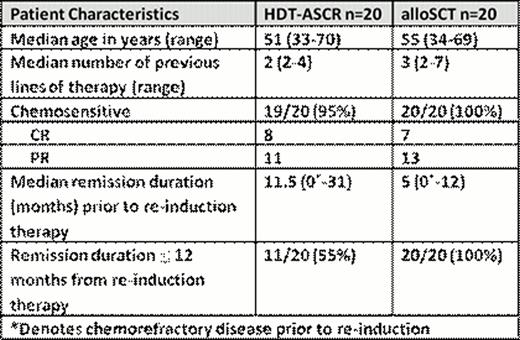
We identified 40 patients with relapsed or refractory FL who had undergone either first HDT-ASCR (N=20) or alloSCT (N=20). All patients had FL grade 1–3a without pathologic evidence of transformation at the time of re-induction prior to transplant consolidation. Patient characteristics are outlined in the table below:
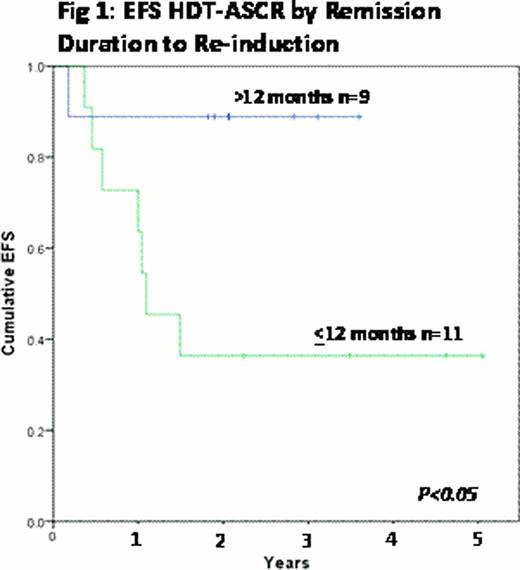
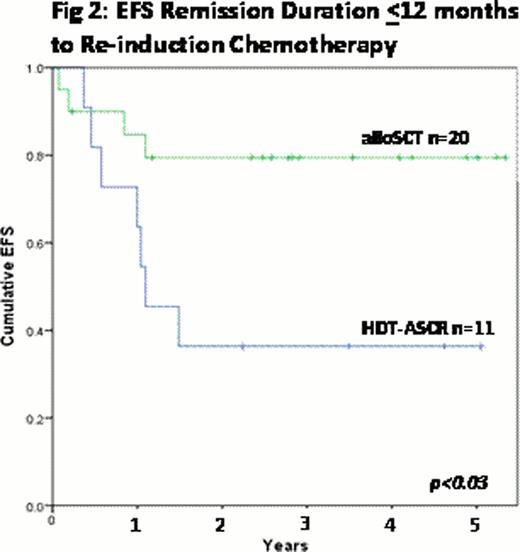
All HDT-ASCR patients received BEAM (carmustine, etoposide, cytarabine, melphalan) conditioning. All alloSCT patients received a uniform non-myeloablative conditioning regimen (cyclophosphamide, fludarabine, total body irradiation 200 cGy). The median follow-up for survivors is 34 months. The estimated 3 year-EFS and OS was 60% and 62% with HDT-ASCR and 79% and 85% with alloSCT respectively (p=ns). FL patients with remission duration ≤ 12 months prior to re-induction therapy proceeding to consolidative HDT-ASCR had significantly shorter EFS compared to those patients with previous remission duration > 12 months (p<0.05, figure 1). Furthermore, when HDT-ASCR and alloSCT patients with a previous remission duration ≤ 12 months prior to re-induction therapy were compared the estimated 3-year EFS was 79% for alloSCT and 36% for HDT-ASCR (p<0.03, figure 2). With relatively short follow-up, there was no difference in OS for these two groups. In the HDT-ASCR cohort eight events were related to progression of FL with three of the eight patients subsequently undergoing alloSCT. In the alloSCT cohort four events occurred with one patient developing DLBCL and three TRM (2-related to graft-versus-host disease; 1-cytomegalovirus infection).
The management of relapsed/refractory follicular lymphoma remains a clinically complex topic. In this exploratory analysis we demonstrated that remission duration of ≤ 12 months prior to re-induction chemotherapy is suggestive of inferior disease control with HDT-ASCR. Longer follow-up is necessary to determine the OS impact. Given the relatively unfavorable pre-transplant characteristics of the alloSCT cohort, FL appears to be exquisitely sensitive to an allogeneic effect. TRM continues to limit the benefit of alloSCT.
Matasar:GSK: Research Funding; Genentech: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal