Abstract
Peripheral T-cell lymphomas (PTCL) are a heterogeneous group of rare malignancies usually occurring in middle-aged to elderly patients (pts), with an advanced disease and unfavorable international prognostic index (IPI) scores. Excluding ALK-positive anaplastic large cell lymphomas (ALCL) and indolent mycosis fungoides, they are often characterized by a poor prognosis. There is no consensus about optimal therapy and the role of allogeneic stem-cell transplantation (allo-SCT) as first line therapy remains to be investigated. In an effort to explore this therapeutic option in younger pts, we undertook a retrospective analysis in 2 french centers.
The records of all pts aged between 18 and 65 years diagnosed with PTCL in Bordeaux and Toulouse between January 2005 and April 2012 were reviewed. Cutaneous T-cell lymphomas and ALK-positive ALCL were excluded. Patients with an IPI score at diagnosis of 0/1 were excluded as well as those who never reached at least a 1st partial response according to the criteria reported by Cheson. Patients relapsing within 3 months after the 1st response and thus ineligible for allo-SCT were also excluded. The primary objective was to compare the outcome of allo-SCT (allo group) as compared to non-allogeneic SCT therapies (no-allo group) in these pts with high-risk PTCL in 1st response.
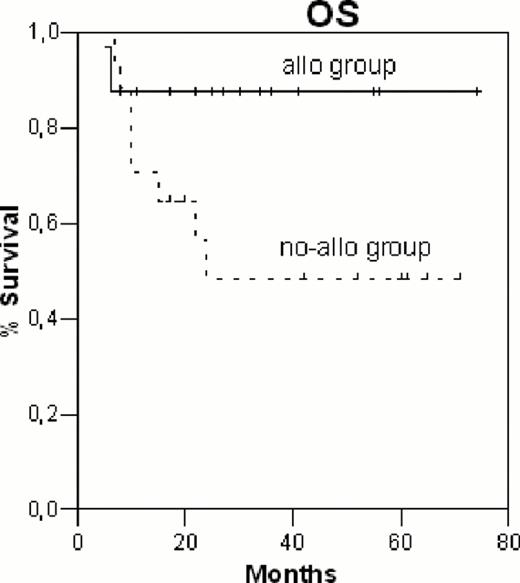
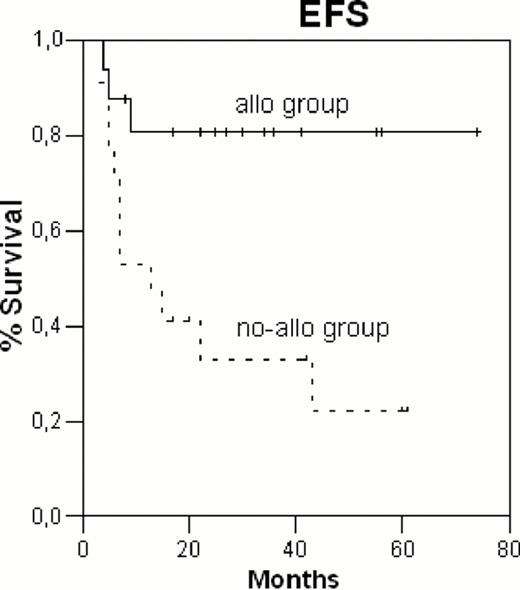
Thirty-three patients were included (16 in the allo group, 17 in the no-allo group). Fifteen pts in the allo group were treated in Bordeaux where allo-SCT was always pursued during the study period in responding pts with an IPI score ≥ 2 at diagnosis. In Bordeaux, the absence of allo-SCT in 1st response was explained by the absence of a suitable donor or the refusal of the patient. The therapeutic strategy in Toulouse was different with 11 pts in the no-allo group, allowing us to undertake this retrospective comparison. In the allo group, conditioning regimes were of reduced intensity (n=12) or myeloablative (n=4). The sources of stem cells were PB (n=13), BM (n=2) or cord blood (n=1). Donors were matched related (n=7), matched unrelated (n=6), mismatched unrelated (n=2). In the whole cohort, the first chemotherapy regimes were CHOP or CHOP-like (n=31), DHAP (n=1), ICE (n=1). In the allo vs no-allo groups, the median ages at diagnosis were 54 years (20–65) vs 59 years (29–64), p = 0.5; the number of pts diagnosed before 2009 were 7 vs 9, p=0.6; the lymphoma subtypes were PTCL-NOS (4 vs 9, p=0.1), angioimmunoblastic (8 vs 6, p=0.4), others (4 vs 2, p=0.3); the IPI scores at diagnosis were 2 (5 vs 5, p=0.9), 3 (6 vs 3, p=0.2), 4/5 (5 vs 9, p=0.2); the number of pts in CR1 and PR1 were 13 vs 13, p = 0,7 and 3 vs 4, p=0.7; the number of chemotherapy lines to reach the 1st response were 1 (8 vs 15, p=0.02), 2 (4 vs 2, p=0.3) or 3 (4 vs 0, p=0.03). Five patients in the no-allo group were treated with an autologous SCT in 1st response. Three patients in the allo group were treated with autologous SCT to reach the 1st response. With a median follow-up of 34 months (8–74) after the 1st response, in the allo vs no-allo groups, the 2-year OS (figure 1) were 87% ± 8% vs 49% ± 13%, respectively (p= 0.06); the 2-year EFS (figure 2) were 81% ± 10% vs 33% ± 12%, respectively (p = 0.007). In the allo and no-allo groups, 3 and 12 pts respectively, have relapsed. In the allo and no-allo groups, 2 and 8 pts respectively, have died, all from disease progression.
The modest size of our study and the potential biases inherent to such a restrospective design preclude the declaration of any firm conclusion. However, these preliminary data suggest that patients under 65 years of age with high-risk PTCL (IPI ≥2) might benefit from allo-SCT in 1st response, in comparison with non-allogeneic SCT therapies. Randomized studies are warranted to further delineate the optimal first line therapy in these patients. Our center is currently participating to such an ongoing european study comparing allo-SCT vs auto-SCT.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal