Abstract
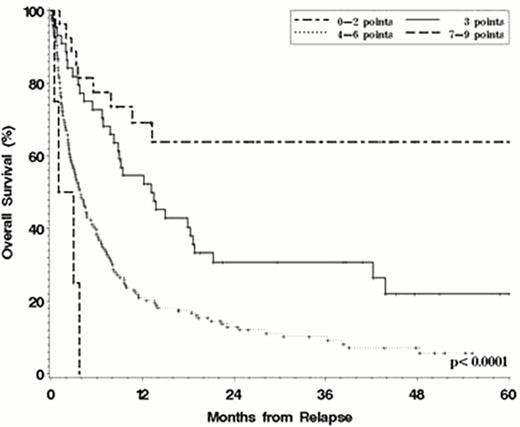
Disease relapse remains a major obstacle to the success of allogeneic hematopoietic stem cell transplantation (HSCT) for patients with hematologic malignancies (HM), and the principal cause of failure after reduced intensity conditioning HSCT. Much work has focused on identifying the risk factors for relapse and devising strategies for its prevention, but comparatively little is known about the outcome of patients who relapse and the relevant prognostic factors in this setting. We conducted a retrospective study of 1080 consecutive adult patients with HM transplanted at our institution between 2004 and 2008. 351 (33%) relapsed at a median of 4.5 months after HSCT. The 4-year post-relapse overall survival (pr-OS) was 15%, with a median post-relapse follow-up of 39 months. Significant risk factors for post-relapse mortality included shorter time to relapse, higher disease risk index1 at HSCT, myeloablative conditioning, and high HCT-CI2 at HSCT. While being on immunosuppression at the time of relapse did not significantly affect outcome in multivariable models, a history of acute or chronic graft-versus host disease (GVHD) prior to relapse conferred a higher risk for death after relapse. Based on those 5 factors and their hazard ratio for mortality in the Cox models, we constructed a simple risk score that stratified patients into 4 groups, with 4-year pr-OS ranging from 64% in patients with fewer than 3 points (13% of the cohort, among whom over one third had myeloid diseases) to 0% in those with greater than 6 points (p<0.0001) (Figure). This score performed similarly in a historical validation cohort of 276 relapsed patients who were transplanted between 1998 and 2003. An analysis of the impact of post-relapse treatment on outcome showed that immune manipulation, through either donor lymphocyte infusion or repeat HSCT, was associated with significantly better pr-OS (4-year pr-OS 28% versus 9%, p<0.0001). Even though this likely reflects in part selection bias, the difference remained significant in models that accounted for other post-relapse prognostic factors, in landmark analyses of patients who survived at least 2 months from relapse, and in patients with active GVHD at the time of relapse. The results of this study may aid with prognostication and management of patients who relapse after HSCT, as well as motivate the design of clinical trials aimed at relapse prevention or treatment in the higher-risk groups.
Post-Relapse Overall Survival by risk score.
Risk factors are:
Disease Risk Index (0 points for low risk, 1 point for intermediate, 2 points for high or very high)1
Time to relapse (0 points for >24 months, 1 point for 6–24 months, 2 points for 3–6 months, 3 points for <3 months)
HCT-CI (0 points for index of 0–2, 1 point for index of 3+)2
Myeloablative conditioning (1 point)
Prior GVHD (1 point)
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
References
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal