Abstract
Abstract 3000
In T effector cells (Teff), protein kinase C theta (PKCθ) is a stabilizer of the immunologic synapse with antigen presenting cells (APCs). Signal propagation through PKCθ leads to activation of inflammatory NF-kB, thus implicating this molecule as a therapeutic target for T-cell mediated disorders as well as GVHD. PKCθ deficiency impairs donor T-cell mediated alloresponse and GVHD while leaving GVL responses intact to a certain extent. Given PKCθ is known to cooperate with its alpha isoform (PKCa) to optimize T-cell signaling and function, we have studied the role of PKCθ and PKCa in T-cell mediated alloresponse after allogeneic bone marrow transplantation (BMT) by using gene-deficient mice as well as a small molecular inhibitor of PKCa and θ.
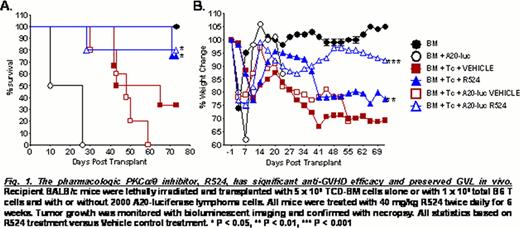
T cells from PKCa, θ and a/θ deficient (−/−) donor mice were tested in their ability to induce GVHD using an allogeneic murine model of myeloablative BMT. GVHD progression was monitored with or without A20-luciferase cells to observe GVL in vivo. To target PKC pharmacologically the small molecule inhibitor R524 (Rigel, San Francisco, CA), specific for PKCa/θ, was tested on GVHD progression in twice daily oral doses of 40 mg/kg for 6 weeks. Efficacy of R524 was assessed in an MHC-mismatched BMT model with and without the addition of A20-luciferase cells and in a minor antigen-mismatched BMT model with or without the addition of C1498-luciferase-DsRed cells to track GVHD progression and tumor relapse.
Using a genetic approach, PKCa−/− donor T-cell alloreactivity is comparable to wild type (WT) T cell responses. WT T cells induced robust GVHD at a dose of 1×106/mouse. The same number of PKCθ−/− and PKCa/θ−/− T cells failed to generate even mild GVHD in recipient mice. At a high T cell dose, 5×106/mouse, PKCa/θ−/− T cells failed to induce severe acute GVHD and increased survival (P < 0.0001). The ability of PKCa/θ−/− T cells to induce GVHD was further reduced from PKCθ-/- T cells as evidenced by greater splenic cell number (P < 0.05) and B220+ B cell reconstitution in PKCa/θ−/− T-cell recipients. B cell activity in PKCa/θ−/− T-cell recipients was greater on a per cell basis; while the activity of T cells isolated from these mice was greatly reduced compared to WT or PKCθ−/− T-cell recipients. Microscopic tissue damage was also reduced (P < 0.05) in GVHD target organs in PKCa/θ−/− T-cell recipients. While not absent, GVL activity was compromised in PKCa/θ−/− T-cell recipients when compared to WT or PKCθ−/− T-cell recipients.
Using a pharmacologic approach, the PKCa/θ small molecule inhibitor R524 reduced (P < 0.05) CD4+ and CD8+ T-cell proliferation (by 44% and 57% respectively) 5 days post allogeneic BMT. Long-term GVHD efficacy studies in an MHC-mismatched BMT model illustrate R524 mediated weight retention (P < 0.002) and decreased mortality (P < 0.01) compared to vehicle treatment. These observations were supported by a reduction in donor T cell expansion (P < 0.05), increased splenic retention of CD4+, CD8+, and B220+ cells and fewer donor T cells found in GVHD target organs of the recipients treated with R524 (P < 0.05). Additionally, CD4+ and CD8+ T cells isolated from spleens, livers and lungs of R524-treated mice produced less CXCR3, CCR6, TNFa and IFNg than their vehicle-treated counterparts. Similar results were obtained from studies using a minor antigen-mismatched BMT model, in which R524 increased recipient weight retention (P < 0.01) and reduced mortality by 50% (P < 0.002). Crucially, GVL activity was largely preserved in R524-treated mice compared to vehicle controls and mortality rates associated with tumor burden were minimal in both MHC-matched and mismatched models of BMT.
In conclusion, we clearly show that PKCa and θ contribute to T cell activity with over-lapping functions in the induction of GVHD and GVL effects. Small molecule inhibition of PKCa/θ signaling with pharmacologic inhibitors presents a valid therapeutic option for GVHD prevention with simultaneous maintenance of GVL activity for clinical consideration.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal