Abstract
Abstract 2893
Monoclonal B-Cell Lymphocytosis (MBL) is a common asymptomatic condition characterized by a clonal B-cell population detected in the blood or bone marrow. The prevalence of MBL is approximately 3–5% in adults over age 40 but rises with age. MBL is a precursor state to CLL and other types of indolent non-Hodgkin lymphoma (NHL). Only a small subset of patients with MBL comes to clinical attention, typically during evaluation for low grade lymphocytosis (designated now as clinical MBL). The rate of progression to CLL requiring treatment among individuals with clinical MBL is ∼1%/yr, and the vast majority of patients with MBL will never develop a B-cell malignancy. Recent data indicate that individuals with MBL are at increased risk of infection similar to CLL. It is unknown whether individuals with MBL are at risk for other adverse outcomes associated with CLL, such as increased risk of non-hematologic cancers (NHC). We investigated the incidence of NHC among patients with clinical MBL and compared this to a cohort of general medicine patients and a cohort of CLL patients.
Mayo Clinic Rochester (MCR) is the primary center for hematologic care in a region including southeastern Minnesota, northern Iowa, and western Wisconsin. No other hematology specialty centers are available within a 50 mile radius of MCR. To explore the risk of NHC in a local, community dwelling cohort of individuals with clinically-identified, CLL-phenotype MBL, we used the MCR CLL database to identify all individuals with newly diagnosed MBL seen in the MCR Hematology Division between January 1, 1999 and December 31, 2009. Analysis was limited to 154 MBL cases residing within 50 miles of MCR. The comparison cohort consisted of 596 adult general medicine patients, with no prior cancer, residing within 50 miles of MCR, who were seen for a general medical exam and enrolled as controls in a case-control study for NHL between April 25, 2004 and December 31, 2009. Rates of NHC in the MBL cohort were also compared to a cohort of 174 patients with newly diagnosed CLL seen in the same time interval as the MBL cohort and also living within 50 miles of MCR. NHC were identified using the Mayo Clinic Cancer Tumor Registry as well as review of medical records in all 3 cohorts. Patients with a NHC diagnosis >3 months prior to the diagnosis date of MBL/CLL were excluded from analysis while those with MBL/CLL and a NHC within 3 months of one another were considered to have a concurrent diagnosis.
There were 125 patients in the MBL cohort, 153 in the CLL cohort, and 596 in the control cohort after excluding patients with prior cancers. The MBL and CLL patients tended to be older (median age MBL=69, CLL=68, Control=58; p<0.0001) and more likely to be male (% male MBL=61, CLL=67, Control=46; p<0.0001) than the controls.
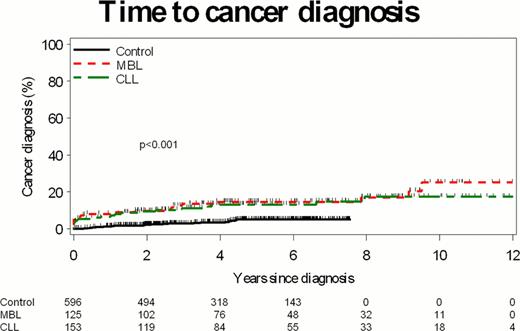
After a median follow-up of 4.2 years (range 0–11), 20 (16%) individuals with MBL developed NHC as compared to 22 (4%) of the controls (Hazard Ratio (HR) MBL relative to control=5.0; 95% confidence interval (CI)=(2.6, 9.4; p<0.0001). Twenty CLL patients (13%) developed NHC, supporting a similar rate to that of MBL patients (HR MBL relative to CLL=1.3; 95% CI=(0.6, 2.5; p=0.49;See Figure). Specifically, the MBL cohort had a higher incidence of cancer of the breast, lung, and nervous system than that of the control cohort. The higher risk of NHC among individuals with CLL and MBL persisted even when patients with “concurrent diagnosis” of CLL/MBL and NHC were excluded (p=0.006) and when patients treated for progressive CLL were censored at the date of treatment (p=0.001)
Finally, we performed a pooled multivariable analysis of all patients (n=874) adjusting for age, sex, major co-morbidities, presence of MBL, and diagnosis of CLL. Age (HR each year older=1.03; 95% CI 1.01–1.06; p=0.003), major comorbidities (HR=1.81; 95% CI 1.07–3.00; p=0.02), CLL (HR=2.10; 95% CI 1.01–4.01; p=0.04), and MBL (2.47; 95% CI 1.30–4.69; p=0.02) were independent risk factors for NHC. The results were similar when the effects of age was modeled in a non-linear (e.g. logarithmic) manner.
In this cohort study, patients with newly diagnosed clinical MBL had a 2.5-fold increased risk of developing NHC relative to the control cohort. MBL was an independent risk factor for development of NHC after adjusting for age, sex, and other comorbidities. This finding adds to the growing evidence that clinical MBL has a distinct clinical phenotype.
Shanafelt:Genentech: Research Funding; Glaxo-Smith-Kline: Research Funding; Cephalon: Research Funding; Hospira: Research Funding; Celgene: Research Funding; Polyphenon E International: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal