Abstract
Detection of minimal residual disease (MRD) has a relevant prognostic value in Acute Myeloid Leukemia (AML). MRD, when used as early treatment response assessment, allows identification of true low-risk and high-risk patients, who may profit alternative chemotherapy approach. In the present retrospective study, we evaluated the impact of MRD assessed by 4-color flow cytometry and WT1 RQ-PCR gene expression in a cohort of AML patients treated at our institution.
Bone marrow samples of 50 adult AML patients (45 de novo and 5 secondary) with available karyotype (K), FLT3-ITD and NPM-A genes mutational status were assessed for MRD after induction. All included patients had a baseline WT1 expression greater than 1000 copies/Ablx104 (range 1060–346060; lab references for normal values 0–500). Fludarabine-based regimen was used as induction; one course of intermediate dose Ara-C 2g/sqm plus idarubicin, followed by 3 courses of intermediate dose Ara-C (2g/sqm) as further consolidation therapy. WT1 log reduction (DWT1) was used to assess the WT1 clearance (DWT1 = logWT1diagnosis – logWT1 post induction). A positive flow MRD was defined by the presence of no less than 25 clustered leukemic cells/105 total events - threshold of 2.5 × 10−4 residual leukemic cells. In patients submitted to bone marrow transplantation (BMT) only the first consolidation course was administered and disease free survival (DFS) was censored at the date of BMT.
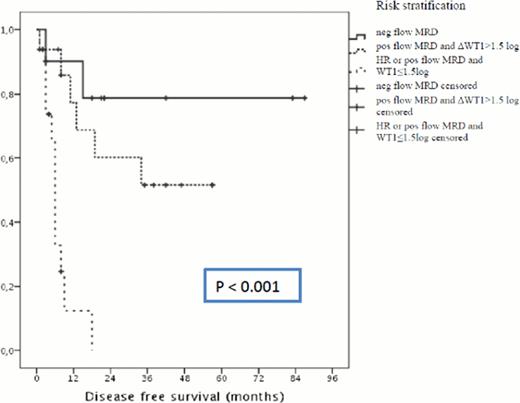
Two (4%) patients had favorable, 40 (80%) intermediate, and 5 (10%) poor risk K (3 had no metaphases); 14 (28/%) carried FLT3-ITD mutation: among them 8 carried NPM-A mutation too, while 6 were wild type. After the first induction regimen 42 of 50 (84%) patients achieved a complete remission (CR). Patients with a negative flow MRD (32%) had 3 years DFS of 69.5%, whereas those with a positive flow MRD (68%) had a DFS of 27.3% (p = 0.032). Patients with a DWT1 > 1.5 log (65%) had a 3-years DFS of 58.3%, whereas those with a DWT1 ≤ 1.5 log (35%) had a DFS at 1 and 2-years of 13,5% and 0%, respectively (p < 0.001). All patients with a negative flow MRD had also a DWT1 > 1.5 log, whereas 12 (52%) of those who achieved a DWT1 > 1.5 log were still positive by flow MRD. Fourteen (28%) patients with a high risk (HR) profile at diagnosis (poor risk K, intermediate K with FLT3-ITDpos/NPM-Aneg, AML secondary to therapy or previous haematological disorder), 6 were no responder to induction, whereas no one of 8 patients in CR reached a negative MRD status in both test with a very poor outcome (projected DFS 4.8 months). MRD assessment using both flow and DWT1 allow to discriminate no-HR profile patients in three prognostic group: good (flow MRD neg) intermediate (flow MRD pos and DWT1 > 1.5 log) and adverse prognosis (flow MRD pos and DWT1 ≤ 1.5 log) with a projected DFS of 70.5 months, 38.2 months and 4.2 months, respectively (p < 0.001).
DWT1 identified patients who would relapse better than flow, whereas a negative flow MRD was the best predictor of long DFS. Using both test in combination with baseline biologic parameters enabled the definition of discrete prognostic categories (Fig 1). Outcome of patients with DWT1 ≤ 1.5 log was very poor and comparable with that of patients with HR profile at diagnosis. In these patients forecast a cure is very difficult with the current treatment option and clinical trials with new drugs should be used already in up-front setting.
Patients in CR after induction: DFS according to baseline biological parameters (HR stand for high risk profile) and MRD assessment. See text for details
Patients in CR after induction: DFS according to baseline biological parameters (HR stand for high risk profile) and MRD assessment. See text for details
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal