Abstract
Acute myeloid leukemia with normal karyotype (AML-NK) is known to be heterogeneous in the molecular level. Accordingly, it has become more critical to dissect this group of patients according to their prognosis using a molecular genetic technology. We attempted to analyze the incidence and prognostic implication of genetic abnormalities on survival in 426 adult patients with AML-NK.
A total of 67 AML-NK patients achieved complete remission (CR), candidate mutations in 21 genes were identified by whole exome sequencing which has 41–89× coverage and by single-nucleotide polymorphism array analysis using marrow mononuclear cells at diagnosis of AML-NK. Subsequently, mutation analysis of 11 genes (i.e. FLT3/ITD, NPM1, DNMT3a, IDH1, IDH2, TET2, NRAS, WT1, DNAH11, SF3B1, and PHF6) which are known to be involved in the pathogenesis of hematologic diseases, were performed using Sanger sequencing in another subset of 359 AML-NK patients as a validation cohort.
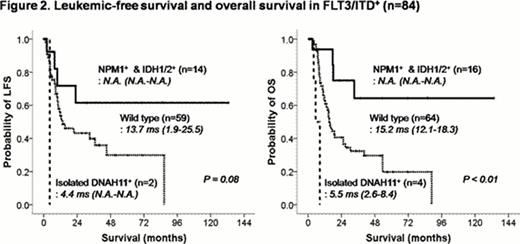
Of 426 patients in total (median age: 51, ranges: 15–85), FLT3/ITD, NPM1, and DNMT3a mutations were associated with higher leukocytes counts at presentation of AML-NK. In 284 patients who received standard remission induction (RI) chemotherapy (excluding 119 patients with conservative treatment and 22 early death/1 follow-up loss after RI chemotherapy), those with FLT3/ITD mutation were significantly associated with a higher risk of relapse (p=0.02), a shorter leukemic-free survival duration (LFS)(p<0.01) or overall survival (OS) (p=0.01). Accordingly, we divided the patients into FLT3/ITD+ and FLT3/ITD− population, and analyzed their treatment outcomes according to the other mutations. In the FLT3/ITD− group (n=200), those with NPM1 mutation showed a higher CR rates after one or two cycles of RI chemotherapy (p<0.01) and a longer OS duration (p<0.01), hazard ratio (HR) 0.43, 95% confidence interval (CI) 0.25–0.73, adjusted by other clinical variables including age, leukocyte counts at diagnosis, and transplantation (Figure 1). In the FLT3/ITD+ patients (n=84), NPM1 mutation was found to be a favorable prognostic factor showing a lower relapse rate (p=0.00), a longer LFS duration (p<0.01, HR 0.35, 95% CI 0.18–0.70), and OS duration (p=0.04, HR 0.55, 95% CI 0.31–0.98) in NPM1 mutated patients. In addition, OS was significantly different in favor of those with IDH2, especially R140Q IDH2 mutation, (p=0.04, HR 0.30, 95% CI 0.09–0.99), whereas DNAH11 mutation was associated with inferior OS (p<0.01, HR 5.78, 95% CI 1.65–20.25). Accordingly, we stratified the FLT3/ITD+ patients into three subgroups according to the NPM1, IDH1/2 and DNAH11 mutation status, Group 1: NPM1 mutation and IDH1 or 2 mutations (n=16), Group 2: isolated DNAH11 mutation (n=4) and Group 3: all mutations were negative (n=64). The group 1 showed significantly better OS than group 2 (p<0.01, HR 16.90, 95% CI 3.48–82.15) or group 3 (p<0.01, HR 3.40, 95% CI 1.20–9.55) (Figure 2). In a subgroup analysis of younger patients less than 60 years of age, similar outcomes were also observed in favor of group 1 in terms of OS (data not shown).
Our study confirmed that NPM1 mutation is an independent prognostic factor in adult patients with AML-NK not harboring FLT3/ITD mutation. In addition, several other genetic markers were identified as prognostic including IDH1/2 or DNAH11 mutations as well as NPM1 mutation in a subgroup of AML-NK patients with FLT3/ITD mutation.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal