Abstract
The optimal timing of hematopoietic cell transplantation (HCT) in AML and its use in risk groups defined by genetic markers or early blast clearance is still under debate. We addressed this question in the AML 2003 study, a large multicenter, randomized, open-label study within the German SAL group. All patients received one cycle of induction therapy (IT) with a 3+7 regimen combining daunorubicin and continuous infusion cytarabine. Upfront cytogenetic and molecular characterization, HLA typing, related donor search and a preliminary search for an unrelated donor were performed for all patients. The subsequent transplant strategy was tailored to the biological risk and donor availability.
Patients aged 18–60 years were randomly assigned upfront 1:1 to either of two transplant strategies: In the control arm allogeneic HCT was scheduled in first complete remission for patients with intermediate risk cytogenetics and an HLA-identical sibling and for patients with a complex karyotype (CK) and a related or unrelated HLA-compatible unrelated donor. In the experimental arm the indication for allogeneic HCT was extended to patients with an FLT3-ITD allelic ratio >0.8 (mutant/wild type), >10% marrow blasts on day 15 after IT1 and patients with adverse karyotypes, including: −7, −5, del(5q), inv(3q), t(3;3), t(6;9), t(6;11), t(11;19)(q23;p13.1). Furthermore, allogeneic HCT was scheduled at an early time-point, i.e. in aplasia after the first or the second cycle of IT in the experimental arm. Patients without an HLA-compatible donor assigned to the transplant strategy were scheduled for high-dose busulfan and cyclophosphamide followed by autologous SCT. Here, we present the final analysis of this study according to the intent-to-treat principle.
Between December, 1, 2003 and November, 26, 2009 1179 patients were randomized between the experimental (N=598) and the control intervention (N=581). The median age was 48 years (range, 18 to 60 years). The distribution of age, ECOG performance status, type of AML, cytogenetic risk groups, NPM1- and FLT3-ITD-mutations, LDH, white blood cell and platelet count was not statistically different between the two treatment arms. However, more males and patients with higher marrow blast counts at diagnosis were randomized to the experimental treatment arm. The median observation time for all patients was 52 months.
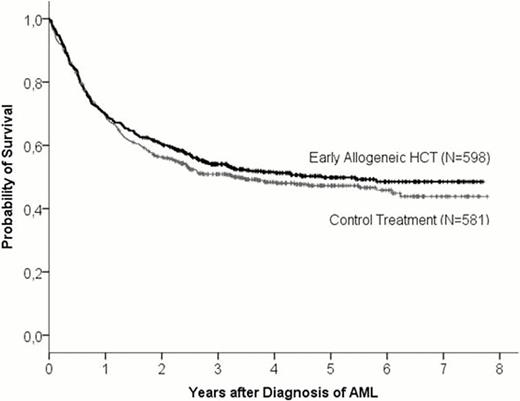
The hazard ratio of the treatment effect (experimental versus control) was 0.92 (95% CI, 0.75 to 1.14; p=0.45) for primary endpoint overall survival and 0.85 (95% CI, 0.71 to 1.02; p=0.08) for the secondary endpoint event-free survival. Patients in both arms had an excellent long-term overall survival of 50% (95% CI, 46% to 54%) at 5 years after enrollment in the experimental arm and 47% (95% CI, 42% to 51%) in the control arm (see Figure). Across all risk groups the rate of early allogeneic HCT performed per protocol was 22% in the experimental arm and 8% in the control arm. Among patients with high risk cytogenetics this rate was 48% and 17%, respectively. These numbers point at the difficulty to deliver allogeneic HCT within two months after diagnosis of AML in the context of a multicenter trial. However, since HLA-typing and preliminary donor search was done for all patients and allogeneic HCT was standard for relapsed or refractory AML in both arms, the rates of allogeneic HCT as first post remission therapy or after induction failure/relapse were substantially higher than in previous studies and almost equal in the experimental and control arm (63% versus 56%).
Although a survival benefit by early allogeneic HCT could not be demonstrated in this large randomized study in newly diagnosed AML, the study treatment resulted in excellent overall survival rates in both arms. Relatively small differences between the per-protocol transplantation rates and crossover effects may partially explain why a benefit of early allogeneic HCT could not be demonstrated. Early awareness of donor availability and the option of allogeneic HCT in patients with primary induction failure or AML relapse resulted in a high overall rate of allogeneic transplantation. This may have contributed to the excellent overall survival in both arms.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal