Abstract
Abstract 2125
Young children typically receive more blood transfusions per kg body weight compared with adults, increasing the risk of iron overload. Iron overload may lead to endocrine abnormalities that can affect growth and development. Data from clinical trials of the iron chelator deferasirox (Exjade®) have demonstrated tolerability and efficacy in transfused patients with a range of underlying anemias. The registration clinical trials included 52 patients aged 2–<6 years who were randomized to receive deferasirox. A 5-year multinational observational registry was initiated to gather further safety and effectiveness data of deferasirox in transfusion-dependent pediatric patients with chronic iron overload.
Patients aged 2–<6 years at enrollment received deferasirox according to local (country-specific) prescribing information. The initial recommended deferasirox dose (ranging from 10–30 mg/kg/day) was based on country-specific prescribing information and adjusted according to serum ferritin levels, therapeutic goals, tolerability and patient weight change. The objectives of this interim analysis were to collect information on renal and hepatic safety; monitoring of serum ferritin levels and investigator-reported adverse events (AEs) was also conducted. Biochemistry analysis, including serum ferritin levels, was based on the full analysis set, and comprised all patients who received ≥1 dose of deferasirox during the registry. The population used for safety analyses comprised all patients who received ≥1 dose of deferasirox and had at least one post-baseline safety assessment. Enrollment is now complete, and study completion is expected June 2015.
As of October 31, 2011, 247 patients (mean age 3.1 years; 1.2% <2 years; 84.2% ≥2–≤4 years; 14.6% >4–≤6 years) with β-thalassemia (n=160, 64.8%), sickle cell disease (n=48, 19.4%), Diamond–Blackfan anemia (DBA; n=11, 4.5%) and other anemias (n=28, 11.3%) were enrolled and received ≥1 deferasirox dose. Patients received deferasirox for a mean ± SD of 30.0 ± 15.2 months. Mean dose was 25.4 ± 6.9 mg/kg/day; 169/243 (69.5%) of these patients had no dose adjustments for a period of ≥1 year, despite a mean percentage weight change of +16.6 ± 12.0% (range −8.9 to 59.1%) during that time. 63/243 (25.9%) had no dose adjustments for a period of ≥2 years and percentage weight increased by +22.5 ± 16.1% (range −1.2 to 72.4%) during that time. At baseline (n=214), median serum ferritin was 1757 ng/mL (range 334–9577), decreasing to 1489 ng/mL (range 156–5102) in patients reaching the 30-month evaluation point (n=57). Mean iron intake was high and remained stable throughout (∼0.6 mg/kg/day).
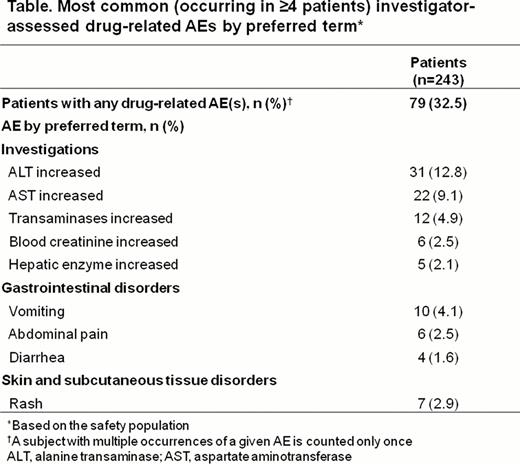
5/247 patients (2.0%) had SCr increases >age-adjusted ULN and >33% increase from baseline on two consecutive measurements (baseline range 20–39 μmol/L); none of these five patients discontinued. Increased ALT >5 × ULN was confirmed in 11/247 patients (4.5%); most abnormalities were transient, five of these patients discontinued (increased ALT [n=3], protocol deviation [n=1] and vomiting [n=1]). The most common (≥4 patients) investigator-reported drug-related AEs were investigations and GI disorders; these are shown in the Table as investigator-reported preferred terms. The majority of investigations were mild-to-moderate in severity.
Overall, 178/247 patients (72.1%) are continuing the study. Main reasons for discontinuation were protocol deviation (n=12, 4.9%) and AEs (n=7, 2.8%: increased ALT; proteinuria; hepatic AE [increased ALT/AST for second time after drug administration]; abdominal pain/vomiting/hypokalemia/transaminase elevation; vomiting; reversible increase of ALT of 239 U/L reported as hepatic cytolysis; transaminase elevation/lack of efficacy; all n=1). One patient with DBA died (severe pancytopenia and sepsis following bone marrow transplantation).
The safety profile of deferasirox in very young pediatric patients was consistent with the available evidence in adult patients, including the rate of creatinine and liver enzyme changes which did not appear to be progressive. Many patients did not have appropriate dose adjustments during the study, despite substantial increases in weight. In addition to safety and efficacy parameters, weight change in pediatric patients should be considered during dose adjustments to optimize efficacy and safety.
Vichinsky:Novartis: Consultancy, Research Funding; ApoPharma: Consultancy, Research Funding; ARUP Research lab: Research Funding. Bernaudin:Novartis: Research Funding. El-Ali:Novartis: Employment. Arrowsmith:Novartis: Employment. Martin:Novartis: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal